| Anatomy |
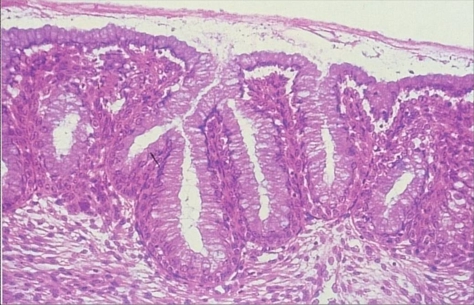
| Endocervical canal |
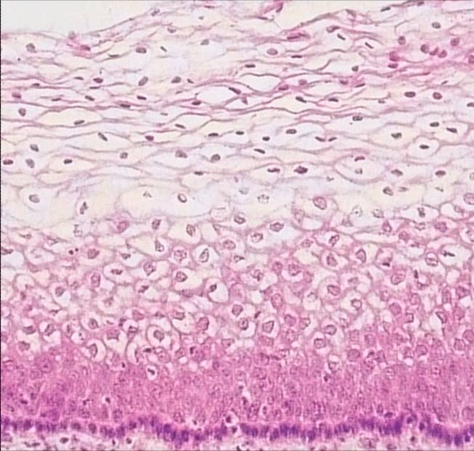
| Ectocervix |
| Squamocolumnar junction, metaplastic process and Transformation zone |
The squamocolumnar junction, metaplastic change and the transformation zone
The squamo-columnar junction is located at the point where the squamous epithelium and the columnar epithelium meet. The location varies throughout a woman’s life due to the process of metaplastic changes in the cervical epithelium which occur after puberty and in pregnancy. The transformation zone is the name given to the area of the cervix comprised of epithelium which has undergone metaplastic change.
Definition of metaplasia
- Metaplasia is the name given to the process by which one fully differentiated type of epithelium changes into another.
- It is usually an adaptive change which occurs in in reaction to longstanding (chronic) irritation of any kind, or in response to hormonal stimuli.
- Metaplastic change is reversible and theoretically transformed epithelium should revert to its original form after the stimulus is removed but this does not always happen.
- Metaplasia occurs at many body sites eg gastric mucosa, bladder,bronchi etc. The metaplastic process has been extensively studied in the cervix.
In the cervix, metaplastic change involves transformation of the endocervical epithelium to squamous epithelium
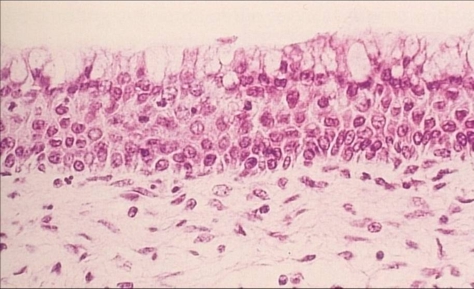
Three histological stages have been identified:
- Stage 1: Reserve cell hyperplasia - the reserve cells in the endocervical epithelium start to divide.
- Stage 2 :Immature squamous metaplasia - the reserve cells proliferate to form a multilayer of undifferentiated cells. A surface layer of mucinous columnar cells can often be seen on the surface.
- Stage 3: Mature squamous metaplasia – the undifferentiated cells have differentiated into mature squamous epithelium which is nearly indistinguishable from the original squamous epithelium.
Metaplastic change in the cervix and its physiological basis
- From birth until puberty the endocervical epithelium is composed of columnar epithelium and the ectocervix of native squamous epithelium. The interface between the two is termed the original squamocolumnar junction.
- During puberty and at the first pregnancy the cervix increases in volume in response to hormonal changes. The endocervical epithelium everts onto the ectocervix (portio vaginalis) exposing it to the acid pH of the vagina. This provides a stimulus for metaplastic change of the columnar epithelium.
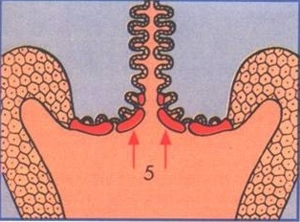
- The process of metaplasia is a patchy one: It starts initially in the crypts and at the tips of the endocervical villae which gradually fuse. Eventually the whole of the everted endocervical epithelium may be replaced by squamous epithelium.
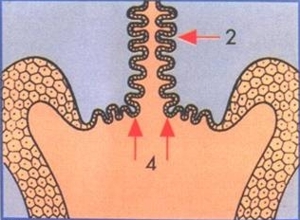
Squamocolumnar junction prior to puberty.
Eversion of the endocervical epithelium at puberty and first pregnancy
Metaplastic change of endocervical epithelium in the transformation zone Relocation of SCJ in the endocervical canal after the menopause Key:
- 1: native squamous epithelium
- 2: columnar epithelium of endocervix
- 3: squamocolumnar junction (SCJ)
- 4: Eversion of endocervical epithelium
- 5: Metaplastic change in transformation zone
Clinical significance of squamous metaplasia in the cervix
In the cervix, the area of the epithelium that has undergone metaplastic change is called the transformation zone (TZ). Numerous studies have shown that the immature metaplastic epithelial cells are susceptible to carcinogens and most, if not all, cervical cancers arise here.
Other forms of metaplastic change in the cervix
Tuboendometriod metaplasia
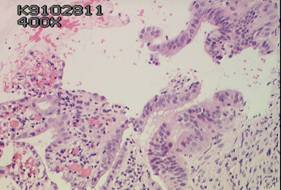
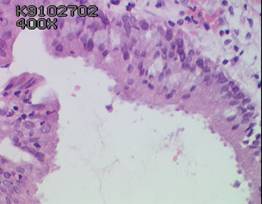
This pattern of metaplastic change often occurs after surgical cone biopsy, diathermy loop biopsy or LLETZ biopsy. Histologically it is characterised by tuboendometrioid glands in the endocervix well away from the uterine isthmus. A key feature of tuboendometrioid change is that there is no associated endometrial stroma The metaplastic epithelium exhibit endometrial features including pseudostratification of the columnar cell nuclei, nuclear hyperchromasia, secretory apical snouting in addition to luminal ciliation.
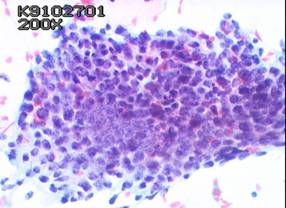
In cervical smears , tuboendometrioid metaplastic changes may be misinterpreted as glandular neoplasia as the cells may form rather ragged crowded groups. However the absence of feathering and rosette formation and the uniform size and shape and the fine chromatin structure of the individual nuclei should permit the correct diagnosis. The presence of a ciliated cell border is diagnostic although a rare finding . ( see also Section on Pitfalls of Diagnosis in Module 10 .)Intestinal metaplasia
This pattern is characterised by the presence of goblet cells in the cervical epithelium and has been found in glandular neoplasms of the cervix.
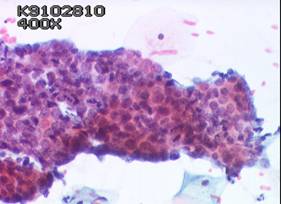
Case 1 Tubal metaplasia of cervix Histology and cytology
Case 2 Tubal metaplasia of cervix Histology and cytology