Cervical Cytology
Anatomy, physiology and histology of the cervix
| Anatomy |
| Endocervical canal |
| Ectocervix |
| Squamocolumnar junction, metaplastic process and Transformation zone |
The columnar epithelium of the endocervical canal
Histological section of endocervical canal Ferning of cervical mucus
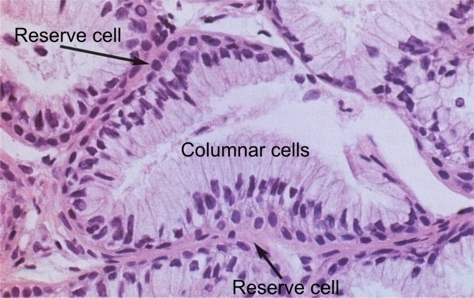
- The reserve cells are small undifferentiated pluripotential cells lying deep to the columnar cells which are more prominent during the metaplastic process.
Columnar epithelium at higher magnification