

Cervical cancer: Epidemiology, aetiology, pathogenesis and main histological types
Clinical presentation of invasive cervical cancer
The clinical presentation and pattern of growth of invasive cervical cancer is variable. The tumour may be have a polypoid or papillomatous appearance or it may be flat or ulcerating. Initially most cancers spread locally- upward into the body of the uterus, downward into the vagina or laterally into the pelvic folds. Eventually the tumour may involve the bladder or rectum and metastatic spread to the liver and other organs occurs. Involvement of the pelvic lymphnodes occurs early in the disease and is associated with a poor prognosis.
The cancers are most commonly diagnosed in women aged 45-65 however they have been described in very young women and an age range of 20-85 has been recorded for these cancers. Women with invasive cervical cancer are often asymptomatic in the early stage of the disease; they may present with post coital, intermenstrual, or post menopausal bleeding, back ache or haematuria when the tumour is at an advanced stage.
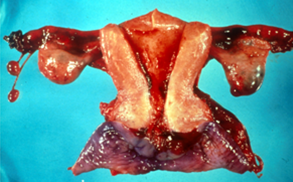 |
| Radical hysterectomy surgical specimen from woman with invasive cervical cancer.The cervix is ulcerated and infiltrated by tumour .Biopsy confirmed invasive squamous carcinoma. |
Staging invasive cervical cancer
Stage |
FIGO: Description |
| 0 | Preinvasive carcinoma (CIN3 or carcinoma in situ) |
| I | Cervical carcinoma confined to uterus (extension to corpus disregarded) |
| Ia | Invasive carcinoma diagnosed only by microscopy |
| Ia1 | Stromal invasion <3mm depth and <7mm horizontal spread |
| Ia2 | Stromal invasion >3mmbut >5mm and <7mm horizontal spread |
| IB | Clinically visible lesion confined to cervix or microscopic lesion >1A2 |
| IB1 | Clinically visible lesion <4cm in greatest dimension |
| IB2 | Clinically visible lesion >4cm in greatest dimension |
| II | Tumour invades beyond uterus but not to pelvic wall or lower third of vagina |
| IIA | Without parametrial invasion |
| IIB | With parametrial invasion |
| III | Tumour extends to pelvic wall and/or involves lower third of vagina and /or causes hydronephrosis or non functioning kidney |
| IIIA | Tumour involves lower third of vagina but no extension to pelvic wall |
| IIIB | Tumour extends to pelvic wall and /or causes hydronephosis or non functioning kidney |
| IVA | Tumour invades mucosa of bladder or rectum and / or extends beyond true pelvis |
| IVB | Distant metastasis |
Treatment of an invasive cervical carinoma
- The clinical staging of invasive cervical cancer is important as it determines the patient’s treatment . Cancers detected at Stage 0 (the preinvasive stage) require only local ablation of the cancerous epithelium, either by diathermy or laser.
- Stage 1 cancers are usually treated by radical hysterectomy with or without preservation of the ovaries according to the patients age.
However in women that have early stage cancer of the cervix, trachelectomy may be used as a fertility saving treatment. A radical trachelectomy is a surgical procedure; whereby the cervix , the upper part of the vagina, the parametrial tissue (tissue around the lower end of the uterus), and the pelvic lymph nodes are removed. The uterus (the womb) and the ovaries are not removed and so it is still possible to have children.
This is done in early cervical cancer; the aim being to preserve fertility. This treatment has been developed in recent years by gynaecological oncologists in specialist centres around the world. It is done vaginally and through small incisions in the abdomen using a laparoscope, (key hole surgery).
- The standard treatments for advanced cervical cancer are radical hysterectomy and/or pelvic radiotherapy.
More advanced cancers may require radiotherapy and /or chemotherapy. The clinical stage at time of diagnosis also affects the prognosis (chances of survival) for the patient.
- The outlook is very good for women with cancer diagnosed in its early stages (Stage 0 or Stage 1) but is poor for women diagnosed with advanced cancer. The prognosis for patients diagnosed at Stage 0 ie the preinvasive stage is excellent with only a very small risk (<less than 1%) of recurrence.
- There is some evidence that cervical cancers in younger women may be more aggressive that those that are diagnosed in women over the age of 40.