

Cervical cancer: Epidemiology, aetiology, pathogenesis and main histological types
The concept of cervical cancer as a multi-stage disease
The concept of cervical cancer as a multistage disease originated at the beginning of the 20th century |
It is widely accepted that most invasive squamous cervical cancers are preceded by an asymptomatic preinvasive stage of the disease in which precancerous cells are confined to the epithelium of the cervix . At this stage, the normal squamous epithelium of the cervix is replaced by an abnormal epithelium composed of neoplastic cells. This is the earliest stage of the disease and is known as cervical intraepithelial neoplasia (CIN). If left undiagnosed and untreated , numerous studies have shown that CIN can progress to invasive cancer. The time span for the progression of CIN to invasive squamous cancer is variable and may be as long as 15 to 20 years. There is strong evidence that invasive cancer can be prevented by the diagnosis and treatment of preinvasive cancer.
Histological studies of the cervical epithelium in women with squamous cancer of the cervix have shown that occasionally an intermediate stage in the development of invasive cancer can be identified .This is termed the microinvasive stage of cervical cancer. At this stage, individual neoplastic cells or small clusters of neoplastic cells can be seen deep to the basement membrane confining the CIN lesion. This is considered to be the earliest evidence of invasion . As the tumour progresses to the invasive stage , tongues of tumour cells extend from the epithelium of the cervix deep into the underlying stroma. The tumour may invade quite extensively locally but untimately invades blood vessels and lymphatic channels leading to metastatic spread.
A preinvasive stage of adenocarcinoma is also recognised histologically and is known as adenocarcinoma in situ or cervical glandular intraepithelial neoplasia (CGIN). The microinvasive stage of adenocarcinoma, although it probably exists, is not a clearly defined histological entity.
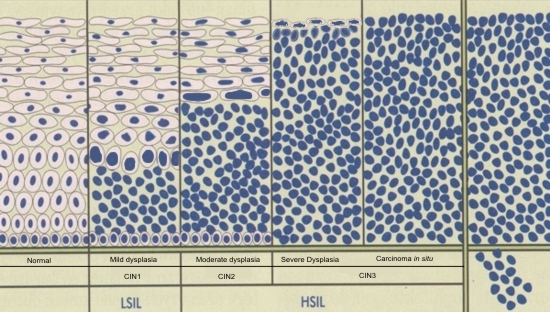
Below is a graphic representation of the stages of development of squamous cervical cancer cancer and shows the progression from normal epithelium through CIN 1 ,CIN2 and CIN3 to microinvasive and invasive cancer. It is probable that most cancers go through these stages although there are reports of cancers arising de novo directly from a focus of CIN1.
-
Preinvasive lesions: WHO and CIN terminology
The concept of cervical cancer as a multistage disease originated at the beginning of the 20th century when Rubin (1910) described histological changes in the cervical epithelium which he believed were precursors of invasive squamous carcinoma. He noted that abnormal cells in the squamous epithelium of the cervix were similar to the tumour cells found in invasive cancer. These changes were subsequently described as “carcinoma in situ “ to indicate the malignant potential of these lesions. Over the next few years, pathologists described a wide range of squamous atypia in the cervical epithelium but there was some uncertainty as to the malignant potential of these changes. The term “dysplasia” was introduced by Reagan et al (1953) to describe the lesser grades of abnormality.The dysplasias were further classified as mild , moderate or severe according to the proportion of the cervical epithelium occupied by the neoplastic cells.
In 1975 the World Health Organisation (WHO) advised that the term “carcinoma in situ “ be used to describe those lesions in which the whole thickness of the epithelium was replaced by undifferentiated neoplastic cells. WHO also recommended that the term “dysplasia” be reserved for neoplastic lesions of the cervix in which only part of the thickness of the epithelium is replaced by undifferentiated tumour cells. It was widely assumed at the time that dysplasia was a pathological condition that was clinically distinct from carcinoma in situ and had no invasive potential: moreover dysplasias did not merit treatment . This assumption was challenged by Richart who subsequently introduced the concept that mild , moderate and severe dysplasia and carcinoma in situ are a lesional continuum in which one abnormality merges into to the next. He introduced the term Cervical Intraepithelial Neoplasia (CIN) as a single descriptive term to embrace all grades of dysplasia including carcinoma in situ under a single disease heading.
Three grades of CIN are now recognised: CIN1 corresponding to mild dysplasia ; CIN2 coresponding to moderate dysplasia and CIN3 coresponding to severe dysplasia and carcinoma in situ. Prospective studies indicated that the risk of progression of CIN to invasive cancer increases with the grade of the CIN lesion .Thus the likelihood of progression is greatest in women with CIN3 and least in women with CIN1.
Both the WHO terminology and the CIN terminology are in current use by histopathologists to describe preinvasive squamous carcinoma .The Bethesda system (TBS) has introduced the terms HSIL and LSIL to describe CIN lesions. These are discussed in the cytology module. The equivalent terminology is shown in Table below.
WHO terminology |
CIN terminology |
TBS terminology |
Mild dysplasia |
CIN1 |
Low grade squamous intraepithelial lesion (LSIL) |
Moderate dysplasia |
CIN2 |
High grade squamous intraepithelial lesion (HSIL) |
Severe dysplasia |
CIN3 |
|
Carcinoma in situ |
CIN3 |
|
Microinvasive squamous carcinoma |
Microinvasive squamous carcinoma |
|
Invasive squamous carcinoma |
Invasive squamous carcinoma |