Cervical Cytology
Anatomy, physiology and histology of the cervix
| Anatomy |
| Endocervical canal |
| Ectocervix |
| Squamocolumnar junction, metaplastic process and Transformation zone |
The squamous epithelium of the ectocervix
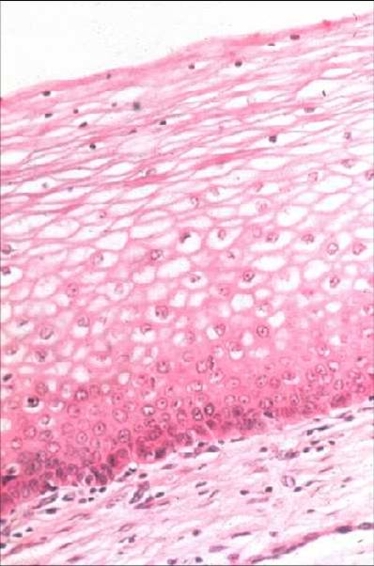
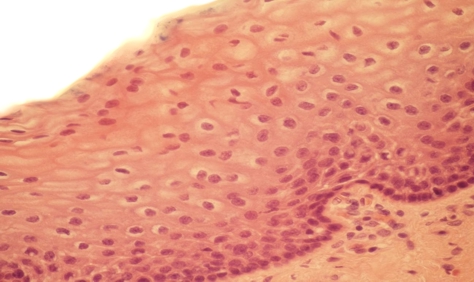
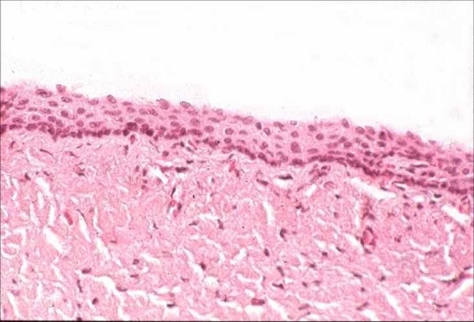
The original squamous epithelium lining the ectocervix is 0.5 mm thick and provides a protective covering for the portio vaginalis of the cervix. It is continuous with the squamous epithelium of the vagina but is less sensitive to hormonal influences than that of the vagina. Its thickness varies with age and with the menstrual cycle – becoming fully mature under the influence of oestrogen but only semi- mature under the influence of progesterone. In the absence of these hormones e.g. after the menopause, the thickness of the epithelium is greatly reduced.
- The mature squamous epithelium consisted of 10-20 layers of epithelial cells which can conveniently be divided into three zones.The basal layer (germinal layer)
- The superficial layer which is made up of the most mature cells.
- The mid or intermediate
- The basal layer made up of squamous epithelium
Histology of the squamous epithelium of the cervix before puberty, during reproductive life and after the menopause:
Squamous epithelium: oestrogen response. Squamous epithelium of ectocervix under the influence of progesterone. Squamous epithelium of ectocervix: after the menopause.