cytologically suspicious follicular lesions
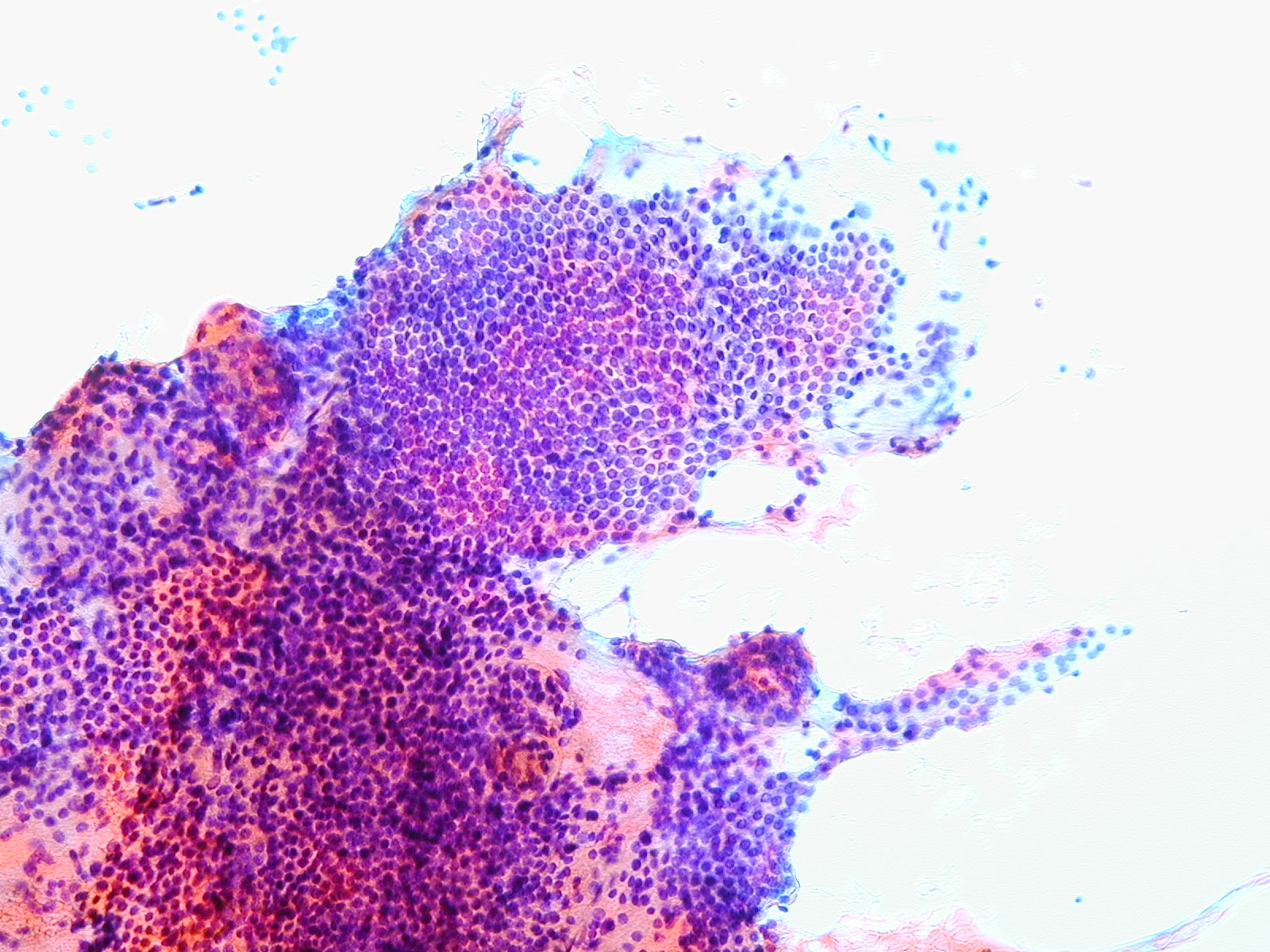
Cytologic diagnostic features
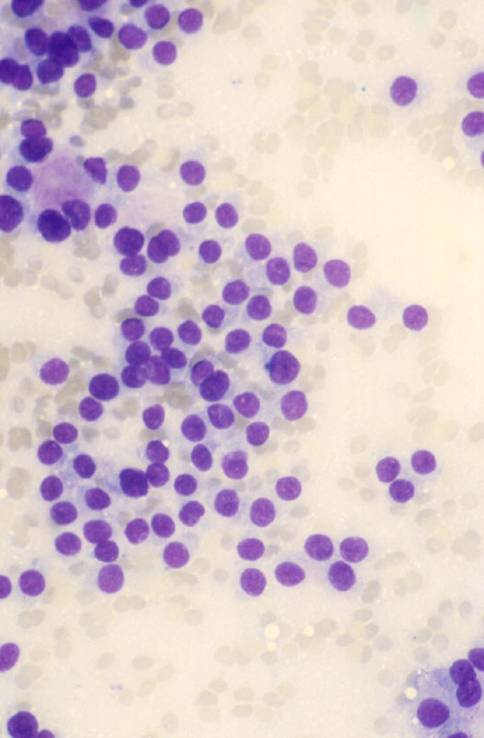
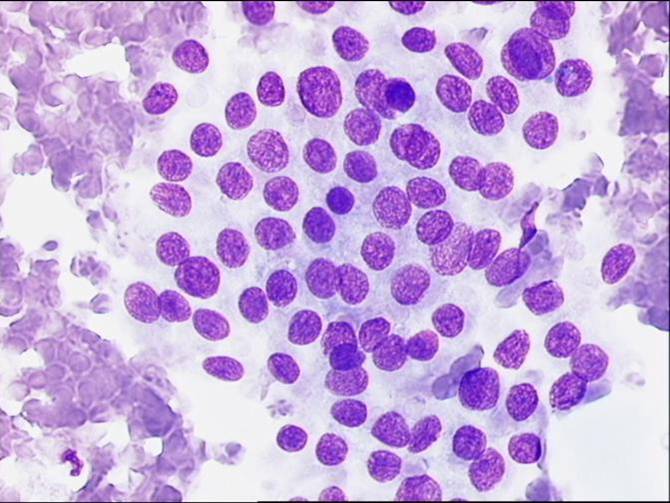
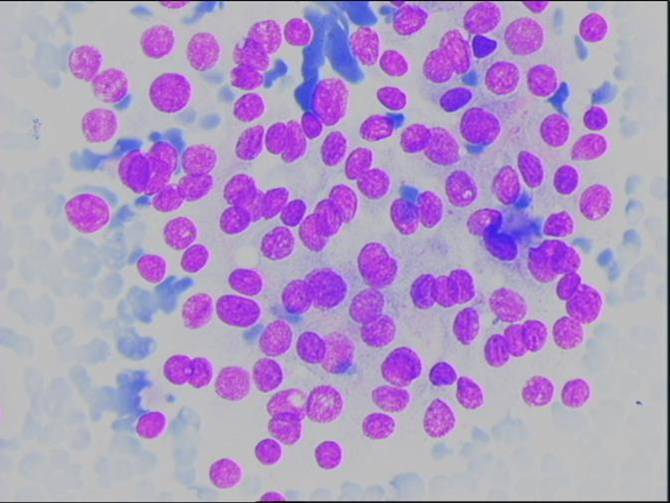
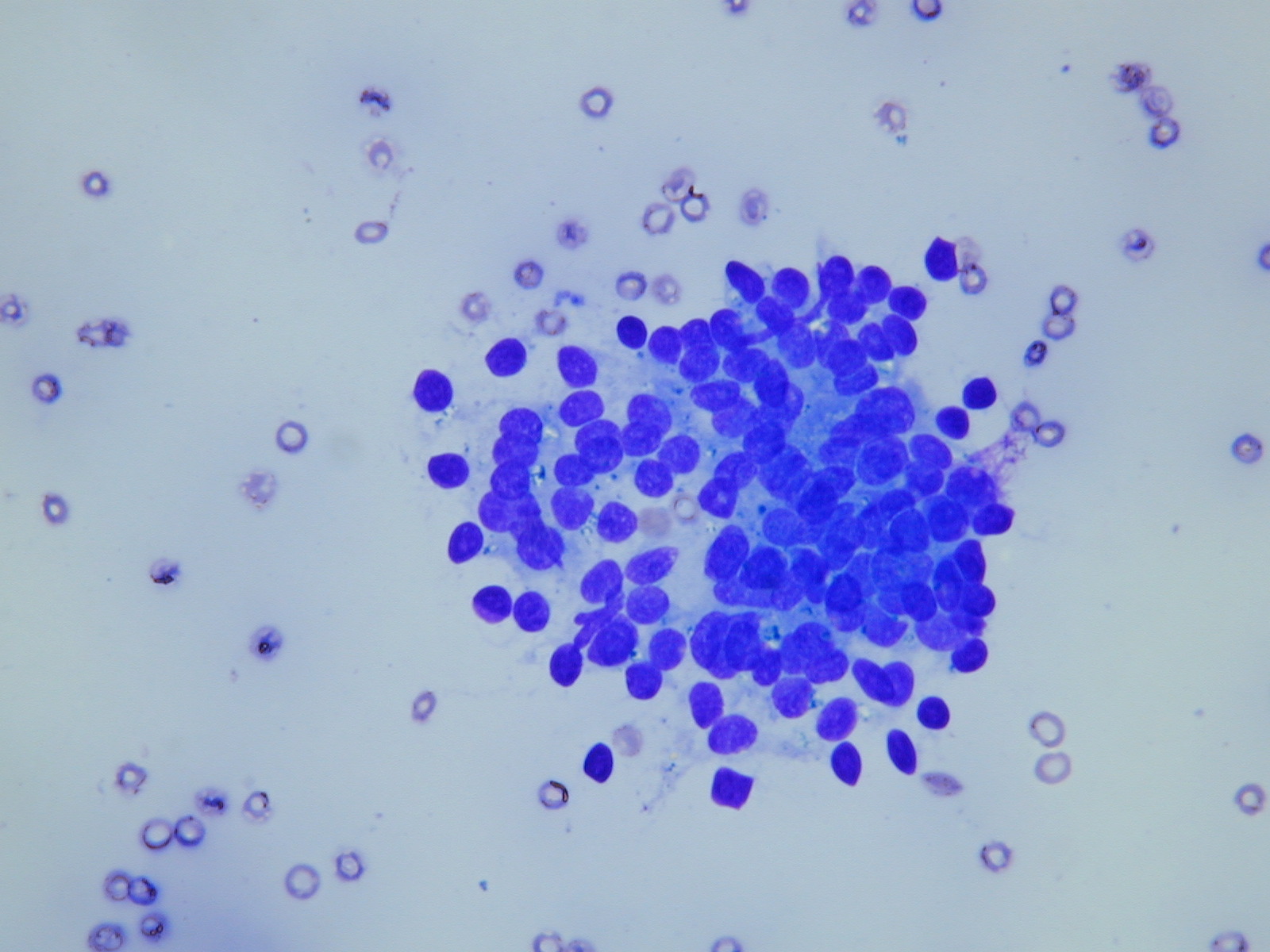
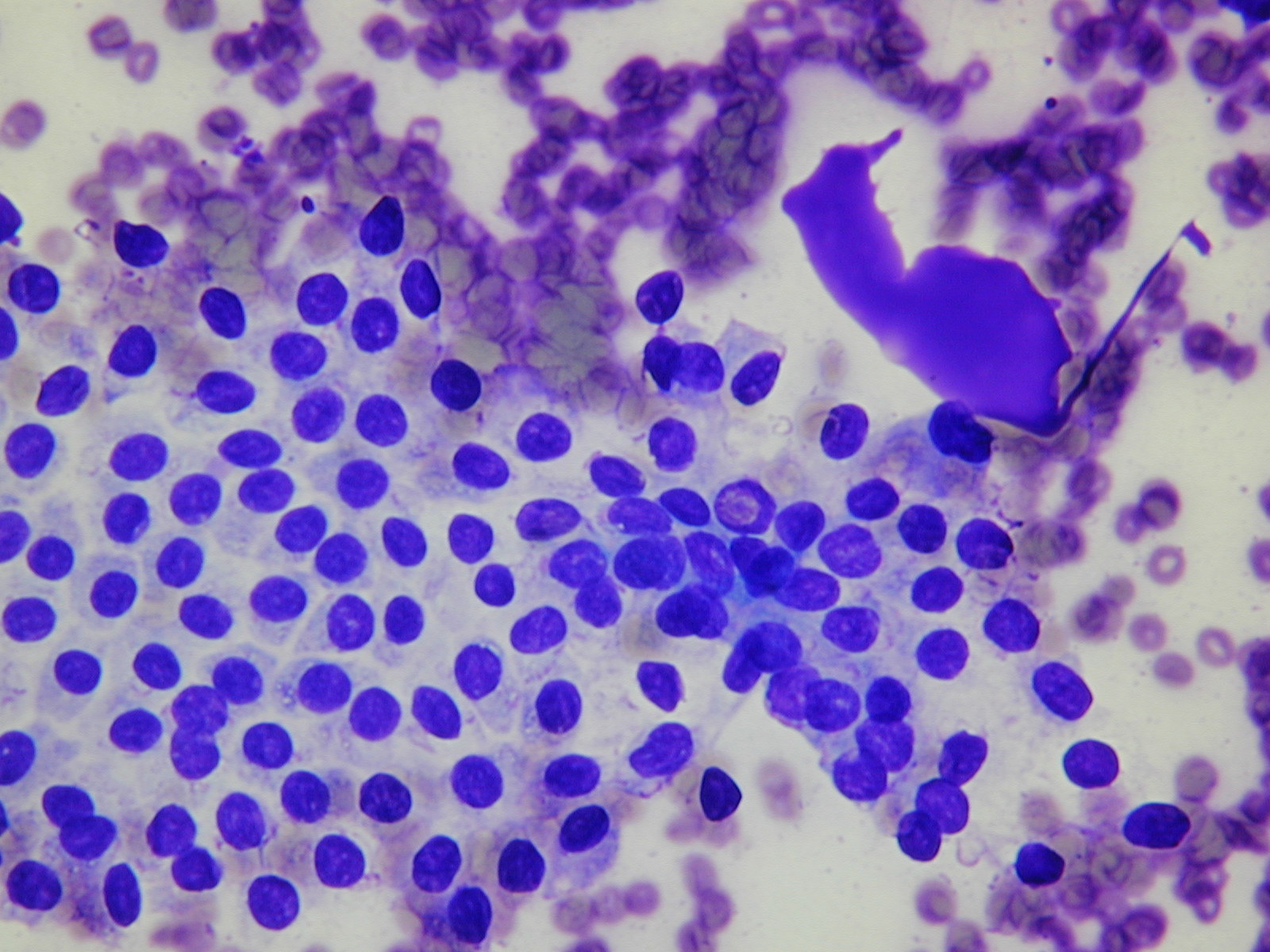
- high cellularity
- predominantly microfollicular or trabecular pattern
- crowded, overlapping cells
- cellular alterations (mild atypia, an uniform enlargement)
- scanty or absent colloid
Several of all of these features should be present to diagnose a follicular lesion as 'cytologically suspicious'. Marked nuclear atypia is uncommon, and so are mitosis. Macrophages are absent. Bare nuclei are usually few or absent.
No single criterion is sufficient to distinguish benign from suspicious nodules. The presence of several features increases the likelihood of malignancy, and that is the case for which a diagnosis of cytologically suspicious follicular nodule should be made. All the aspirates that are composed of a pure Hürthle cell population are suspicious by definition.
The differential diagnosis includes other thyroid neoplasms. Nuclear grooves and pseudoinclusions may be focally present in some follicular adenomas and carcinomas. If focal, they should not lead to a diagnosis of papillary carcinoma but will define the lesion as supicious. In the so-called hyalinizing trabecular adenoma, smears show oval or spindle cells in aggregates or isolated. Clues to the correct diagnosis are a whorling, parallel array of the cells, an amorphous hyaline material and a perinucleolar clear zone. The clear cell variant of follicular carcinoma may be confused with some parathyroid tumors or metastatic renal cell carcinoma, but cells are usually positive to immunostaining for thyroglobulin.
Only about 30-40% of cases diagnosed as 'suspicious follicular nodules' prove to be malignant. Among these, only 50-75% are follicular carcinomas, while the others prove to be follicular variants of papillary carcinoma.
The Thy classification has been devised clinically to separate lesions at higher risk of malignancy from the ones with a low risk. In both cases the surgeon will offer excision of the nodule but will point out that in the former (Th4 category) the risk is approximately 80% while in the latter (Th3) is approximately 20%.
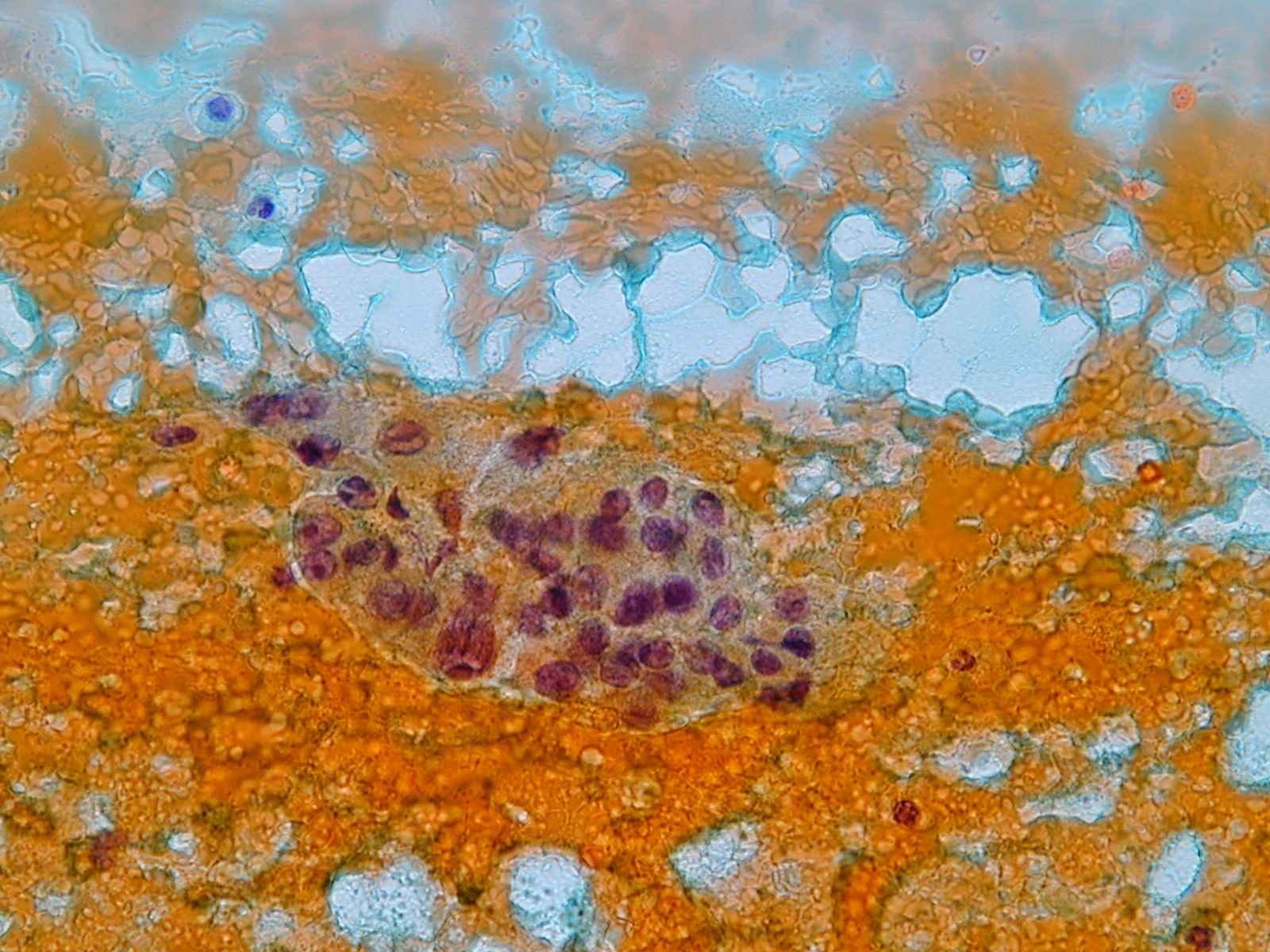
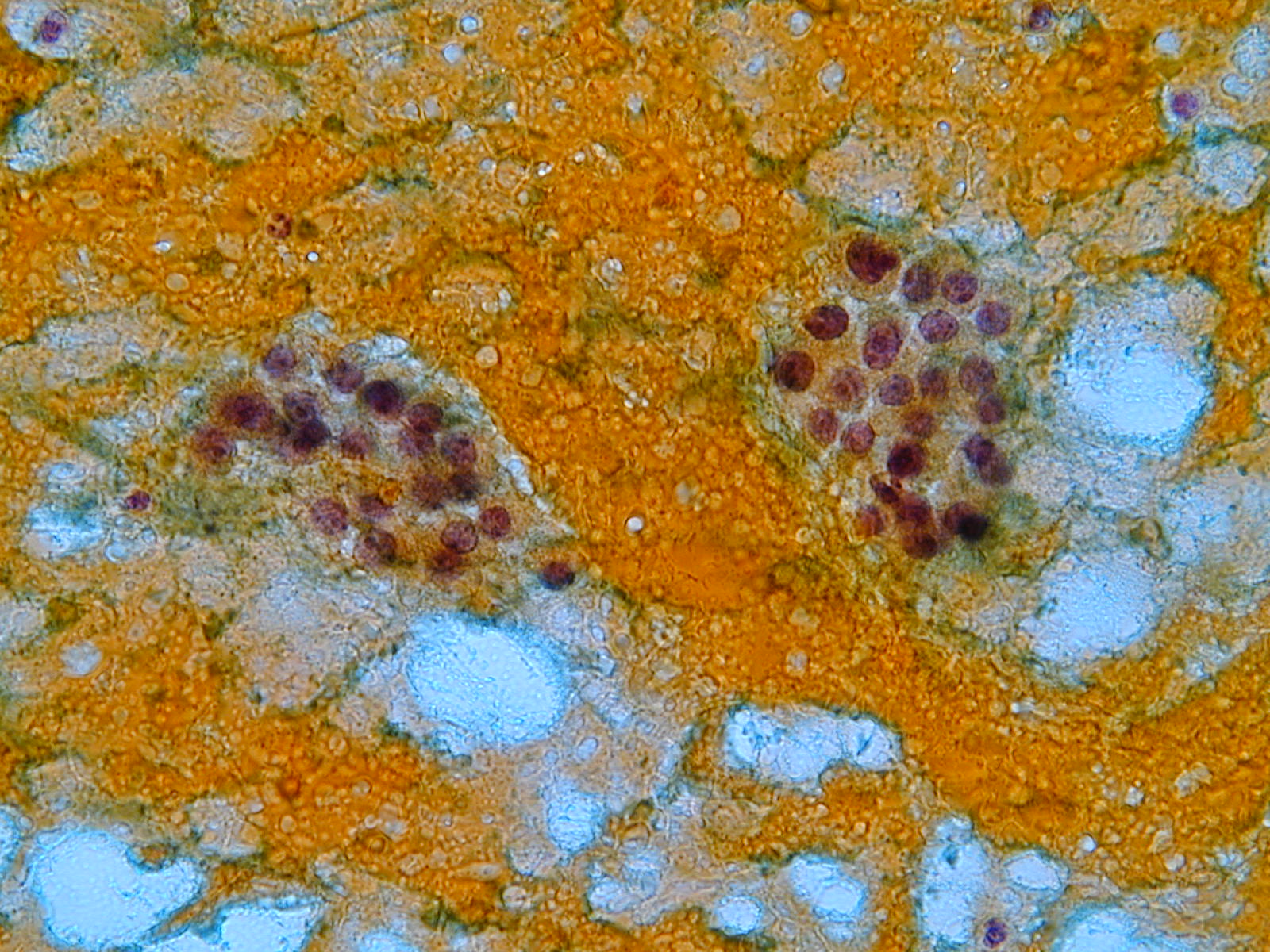
In patients with a diagnosis of 'suspicious follicular nodule' a lobectomy is usually performed; if a carcinoma is diagnosed by the hystological examination, a complete thyroidectomy is recommended.Adjunctive techniques have been advocated to discriminate between benign and suspicious follicular lesions. Morphology and image analysis proved not to be sufficiently accurate for clinical purposes. DNA measurements by flow cytometry is also not useful; in fact, aneuploidy does not guarantee that a tumor is malignant. Immunocytochemistry for MIB-1 is not of great value, since the proliferative activity in adenomas and carcinomas can be similar. Immunocytochemistry for galectin-3 appears to be promising, since most carcinomas are positive and most adenomas are negative, but is not specific or sensitive enough in clinical practice. The distinction could be made also with genetic markers: the translocation t(2;3) is a specific marker of follicular carcinoma.
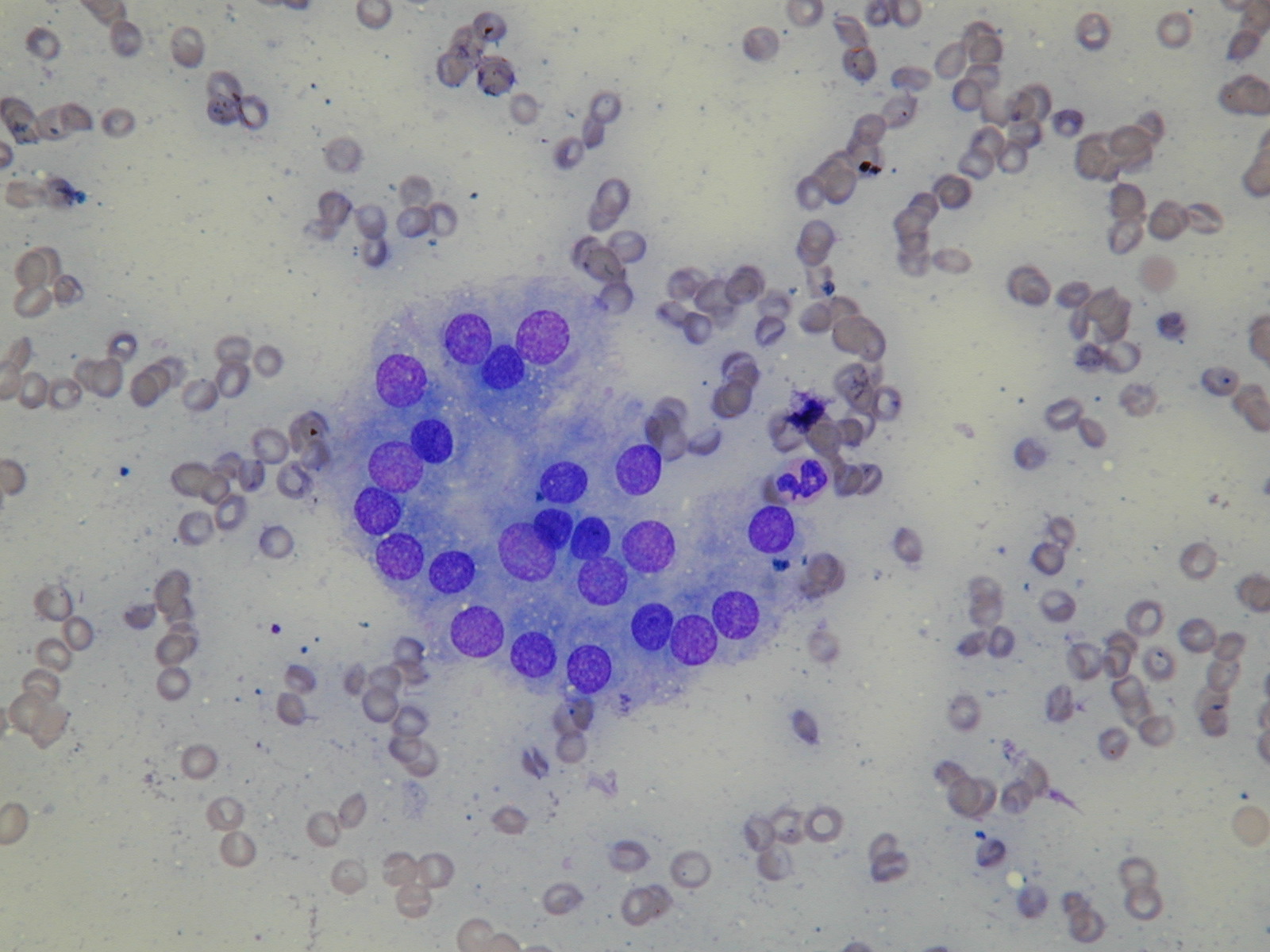
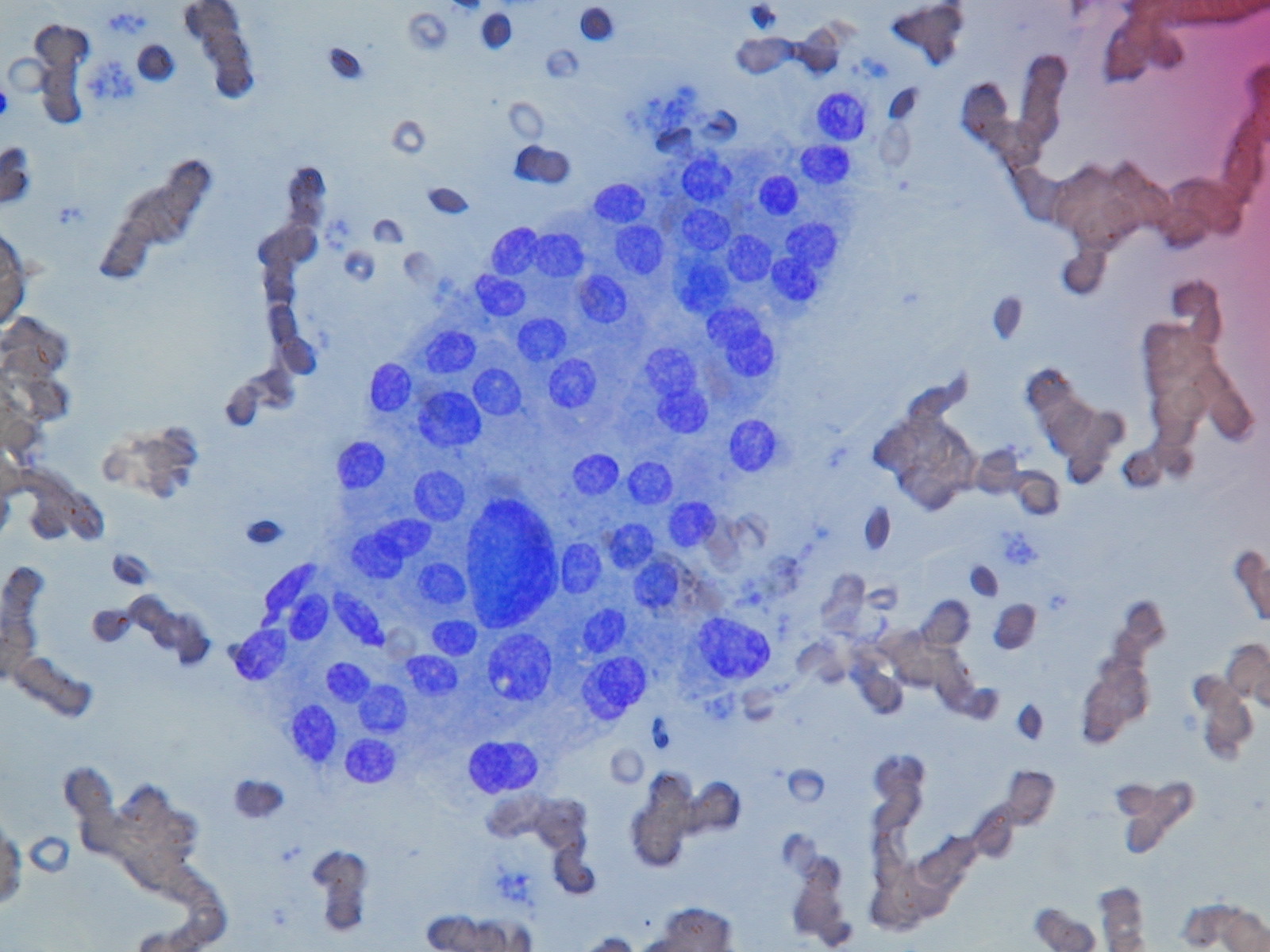
A group of cells with marked anisonucleosis. A central nucleus is much larger, hyperchromatic and has an irregular contour .