Anatomy
The thyroid is an endocrine organ situated in the neck. Its position, close to the thyroid cartilage gave the organ its name as thyroid is derived from the Greek word ‘thyros’, meaning shield – it was originally considered to protect the larynx. Embryologically the thyroid develops at the base of the tongue from the fusion of three structures and descends from there during gestation to its final position in the anterior neck.
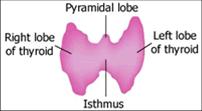
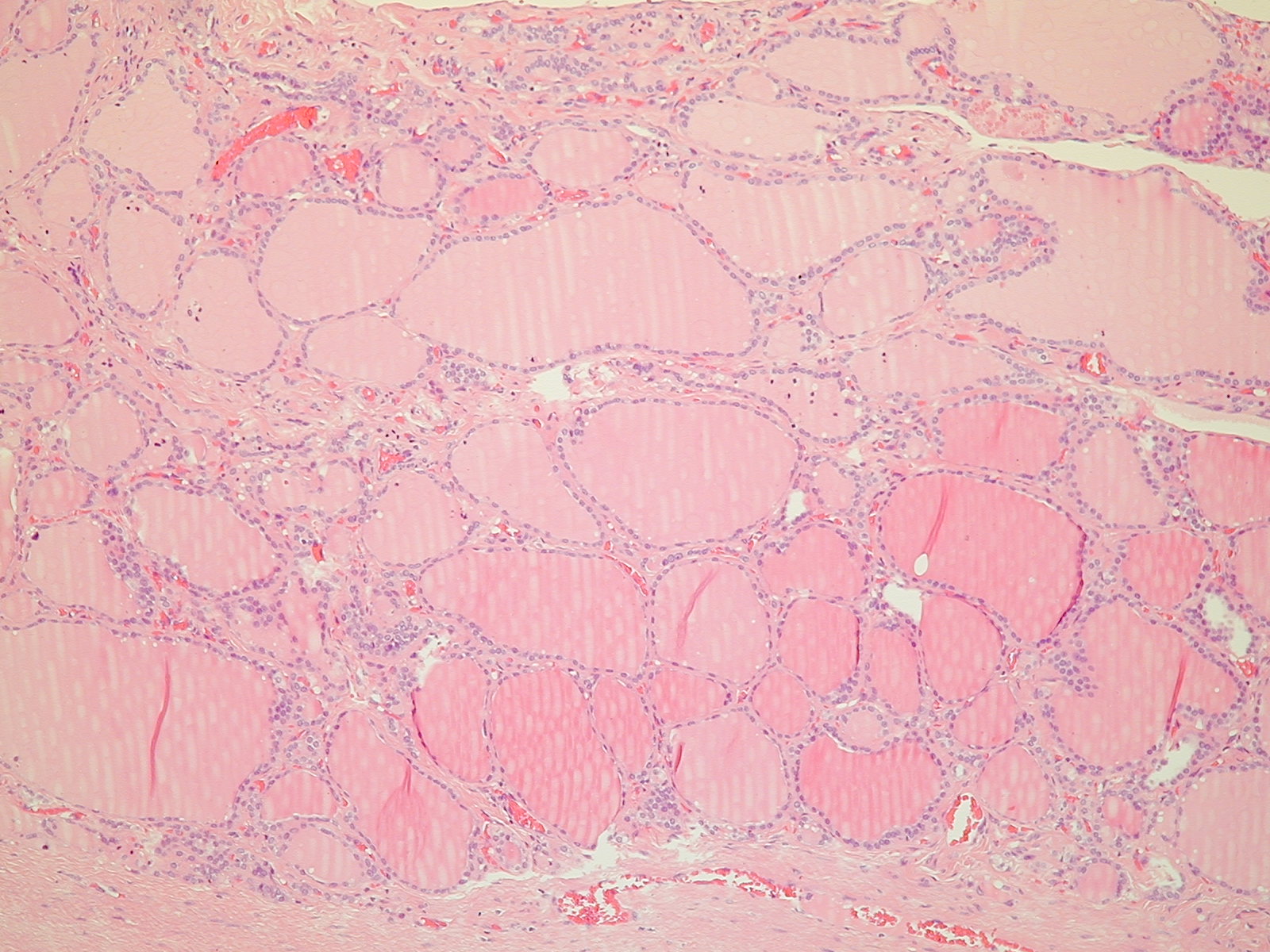
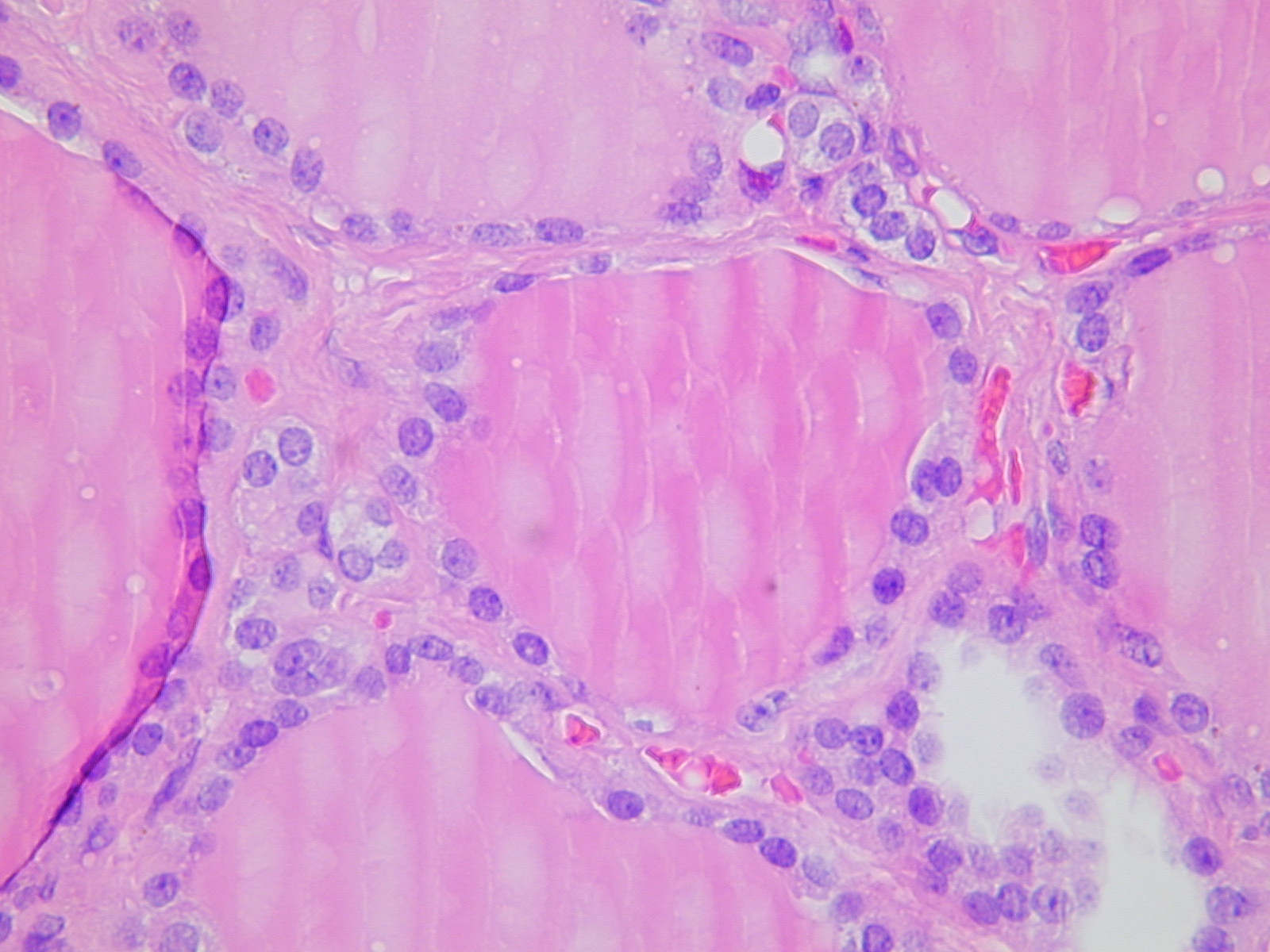
The mature thyroid consists of two lateral lobes joined by an isthmus and enveloped by a thin capsule. The parenchyma of the thyroid is subdivided by fibrous septa into lobules each of which consists of numerous functional units known as follicles. Each follicle is lined with cuboidal follicular cells and is filled with thyroglobulin-containing colloid. The thyroid is highly vascular and has a widespread network of capillaries and arteries which surround and supply individual follicles. Each follicle is enclosed by basement membrane between which are parafollicular cells containing calcitonin (secreting C cells). The two types of cells can be easily distinguished especially by electron microscopy as they are morphologically different. Follicular cells have a basal nucleus with homogenous chromatin and the rough endoplasmic reticulum is well formed. There are also apical secretory vesicles and small mitochondria present. The C cells in contrast show numerous neurosecretory granules containing calcitonin.
Physiology
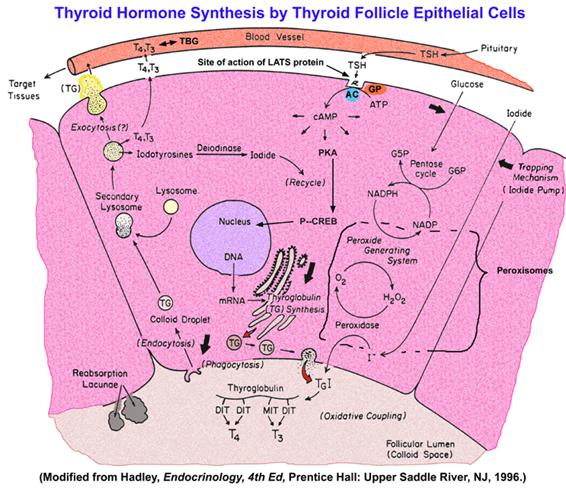
The thyroid hormones T3 (tri-iodothyronine) and T4 (thyroxine) are synthesised within the gland. More T4 than T3 is produced but T4 is converted to its more active form, T3, in some peripheral tissues such as liver, kidney and muscle by a deiodination reaction. The synthesis of these involves the concentrating of iodine by the follicular cells using a Na+-K+-ATPase pump (the iodide trap). Once inside the cells the iodine is rapidly oxidised to a more reactive form. This is then organised by linking to tyrosine amino acids to form thyroglobulin. Prior to the secretion of the thyroglobulin into the colloid it undergoes a coupling reaction to form T3 and T4 which remain attached to the protein. When the follicular cells are stimulated by thyrotrophin (thyroid stimulating hormone or TSH) from the pituitary, colloid is taken into the cells by endocytosis where enzymes degrade the thyroglobulin and release the iodinated units. The control of TSH release is regulated by another hormone called thyrotrophin releasing hormone (TRH) which is synthesised and secreted from the hypothalamus. The overall control of this entire system occurs via a negative feedback mechanism with T3 and T4 acting on the pituitary and hypothalamus to prevent or restrict the release of TSH and TRH respectively.
When the T3 and T4 are released into the circulation, they combine with plasma proteins, mainly thyronine binding globulin (TBG). Less than 1% of these iodothyronines are free in the circulation – this is the active portion. The actions of T3 and T4 in the periphery include increasing the basal metabolic rate of most cells in the body, increasing lipolysis and carbohydrate metabolism, potentiating the effect of catecholamines on the heart and central nervous system and increasing protein metabolism, particularly degradation. From this list it is clear that with any imbalance of the thyroid hormones such as in hyper- or hypo-thyroidism there will be drastic effects on the body.