Diagnostic tests in thyroid nodules
Clinical history and examination are the first step to approach the investigation of the thyroid nodule; however they are not sufficiently accurate by themselves. Ultrasound examination, which can discriminate between a solid and a cystic nodule, does not reliably predict malignancy. Radionuclide imaging is not useful to identify malignant lesions: most carcinomas appear as “cold” nodules (inefficient at trapping iodine) but so do benign nodules, while hot nodules are almost always benign. FNA proved to be by far the most valuable test to identify patients with thyroid cancer, significantly reducing the number of patients undergoing surgery.
Thyroid FNA was introduced by Soderstrom in 1952 and by 1980 the Karolinska Institute in Stockholm had accumulated an experience of >20,000 cases. It is simple, safe and accurate method of diagnosing malignant thyroid conditions and by far the most cost-effective diagnostic test. The overall sensitivity averages about 83% and specificity about 92%. However these figures can be significantly increased when the cytopathologist directly performs the FNA himself and immediately assesses the material.
Indications of FNA
The main indication for FNA is a solitary nodule or a dominant nodule in a multinodular goiter. Only a small percentage of the nodules are malignant (about 5%). Malignancy is most likely in the folowing conditions: age < 20 or > 70, male sex, history of neck irradiation, family history of thyroid cancer or MEN type 2, firm, irregularly shaped and fixed thyroid gland, cervical lymphadenopathy.
Aspiration technique
The aspiration, which can be guided either by palpation or ultrasonography, is performed when the patient is either supine or sitting with the neck hyperextended. Asking the patient to swallow may facilitate the localization of the nodule while holding it with one hand.
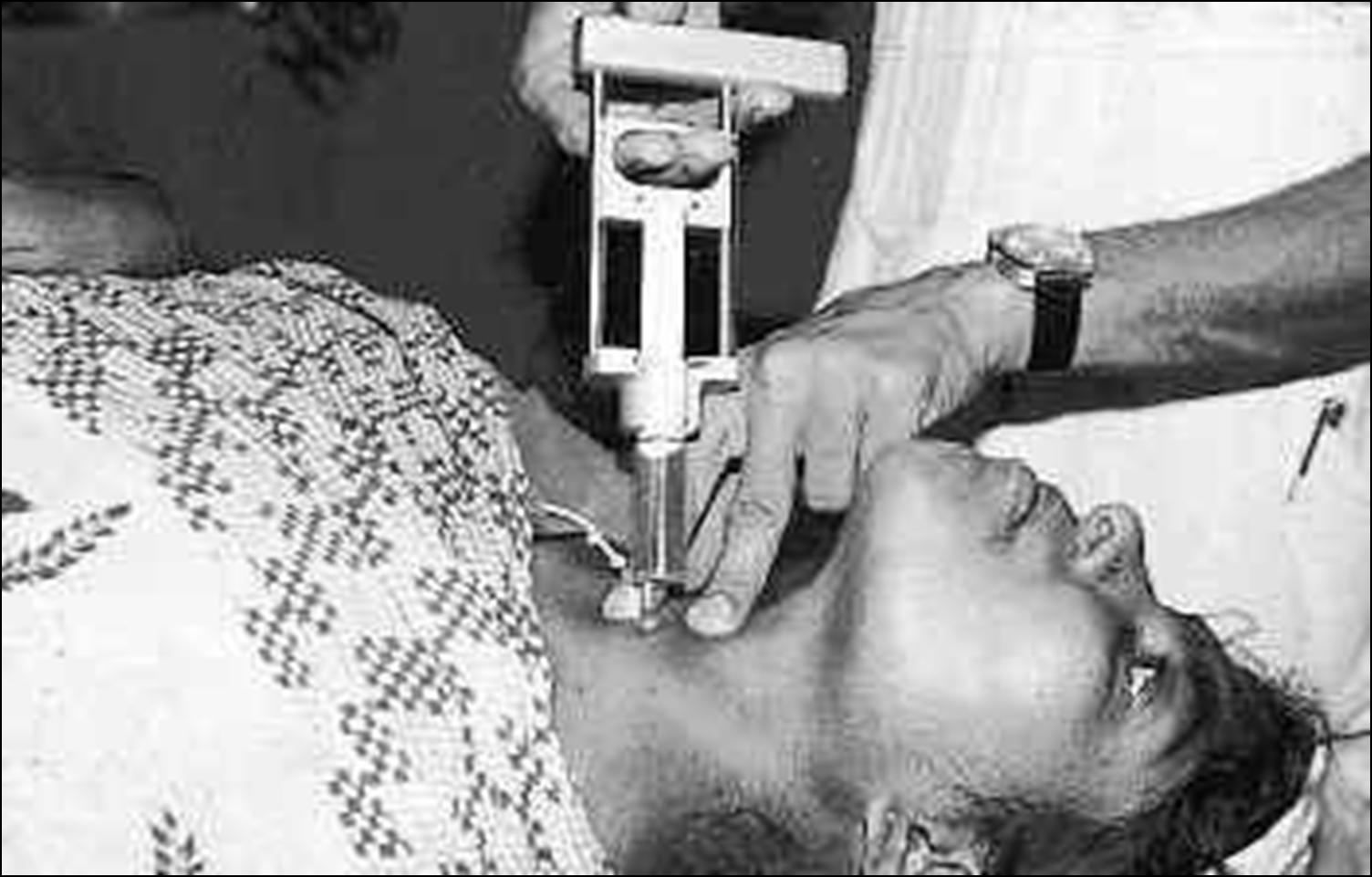
A small needle (25-27 G) is inserted at the periphery of the nodule, which is sampled with an up and down movement; the needle is rotated and then extracted as soon as blood appears. The patient should not swallow during the procedure. The use of a very fine needle is painless (no anaesthesia is needed) and reduces bleeding, avoiding contamination of the specimen with blood and so improving its quality.At least two passes will be made; a cytopathologist should be present to evaluate the specimen for adequacy, if not directly performing the aspirate. If a cyst is aspirated, a residual solid area will be sampled. Only if the nodule appears calcified or fibrous a repeat aspiration should be performed with Franzen’s pistol (syringe holder).
A patient undergoing thyroid FNA via the non-aspiration technique (needle only). A patient undergoing thyroid FNA via the aspiration technique (with Franzen' s pistol - syringe holder). Slide preparation
The cells are expelled and smeared onto a slide. As an adjunct to smears, the needle should be rinsed out and placed in a container. The suspension can be used for cytocentrifugation, thinlayer or cell block preparations. The advantages of thinlayer preparations over smears include reduced blood and decreased screening time, but adjustment to mild alterations in cellular appearance is necessary. Smears can be alcohol-fixed and Papanicolaou stained or air-dried for Romanowsky-type staining. Nuclear features are better appreciated with the Papanicolaou stain, while Romanowsky-type stain is useful to evaluate cytoplasmic details and extracellular material, such as colloid.