| Introduction |
| Technical aspects |
| Normal lymph node histology and cytology |
| Reactive lymph node |
| Hodgkin Lymphoma |
| Non Hodgkin lymphoma |
| Metastases |
METASTASES
Clinically evident metastatic lymph nodes are generally characterized by diffuse involvement; hence, FNC is diagnostic in most cases;when the primary tumour is unknown, FNC may contribute to its identification. As in case of lymphomas, the immediate evaluation of the smear may require additional passes, can orientate the management of the diagnostic material and lay out an immunocytochemical panel combining cytological features and clinical data. If the primary tumour is known, FNC may produce a definite diagnosis using routine smears. Differentiated metastatic tumours show, in most of the cases, quite indicative cytological features: papillary thyroid carcinoma, melanoma or breast carcinoma may be typical enough to suggest their histogenesis at FNC. Even some poorly differentiated tumours, such as undifferentiated pharynx tumours or lung carcinoma, for their peculiar cytological features are often typical enough to suggest the primary tumor.
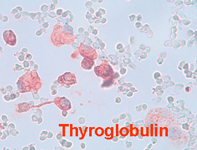
Metastases from unknown tumours are approached in different ways in different districts. In cases of breast tumours, pre-surgical FNC assessment of axillary lymph nodes has become less significant since they are surgically investigated during surgery. Conversely FNC of clinically evident axillary lymph nodes may reveal metastases of unknown and sometimes undetectable breast tumours. Papillary thyroid carcinoma may cause precocious lymph nodal metastases; thyroglobulin measurement in FNC wash-out, combined with traditional smears may be useful to diagnose lymph node metastases of papillary thyroid cancer. Tyrosinase reversetranscriptase polymerase chain reaction of aspirates obtained by ultrasound-guided FNC of sentinel nodes has been utilized in patients with melanoma to detect occult metastases, with different degrees of diagnostic accuracy.
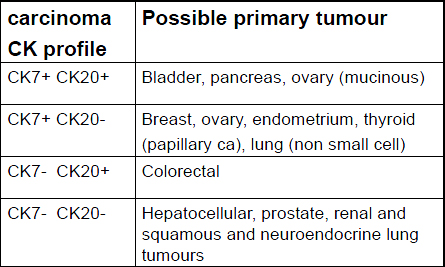
In most cases, a basic immunocytochemical panel combining two or more antibodies may suggest the primary tumour (see tables I and II). In this perspective both cytospins and cell blocks generally produce a sufficient number of slides, and cell blocks allow the testing of different antibodies on the same cell groups.
Table I: basic antibodies for tumours identification
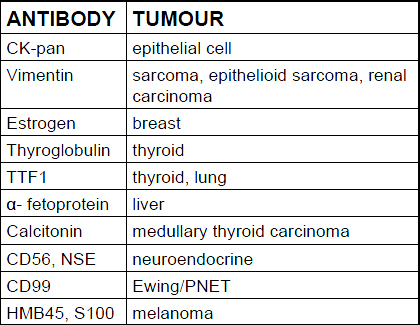
Table II: cytokeratins expression in epithelial tumours
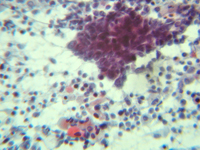
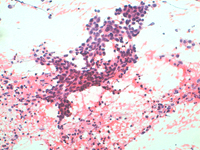
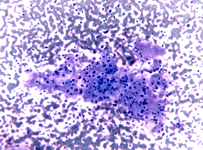
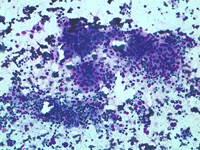
Squamous cell carcinoma
Lymph-nodal metastasis from squamous cell carcinoma may show variable cytological presentations; thick groups of poorly differentiated cells, differentiated squamous malignant cells, “tadpole” cells and abortive corn pearls may be intermingled with lymphoid cells or in a necrotic background.
Squamous cell carcinoma
Lymph-nodal metastasis from squamous cell carcinoma showing groups or isolated squamous cells with atypical nuclei and different degree of differentiation. In some cases a necrotic or suppurative background may simulate an inflamatory process.
Lung adenocarcinoma
Groups of epithelial cells organized in balls or dense groups with scattered lymphoid cells in the background.
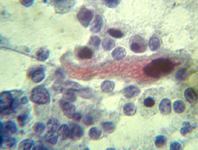
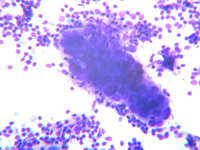
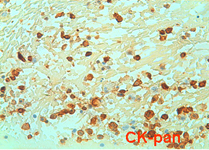
Undifferentiated rinopharinx carcinoma
Rinopharinx, carcinoma may cause precocious lymph-nodal metastases; in most of the cases later cervical lymphnodal metastases are the first sign of the disease. Small groups of poorly differentiated cells or isolated undifferentiated cells, cytokeratin positive, represents the typical presentation of lymph nodal involvement.
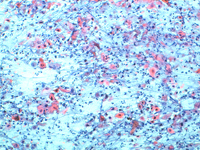
Renal carcinoma
Lymph nodal metastases from renal carcinoma may be suggested by large, isolated cells with wide clear and or vacuolated cytoplasm or by large groups of cells with “oncocytic” large cytoplasm and bland nuclei.
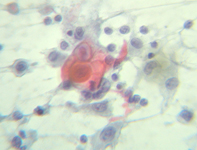
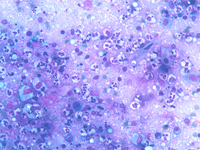
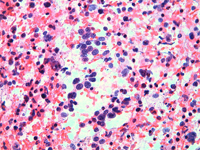
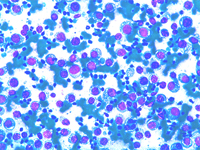
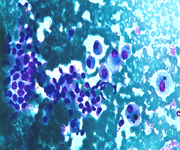
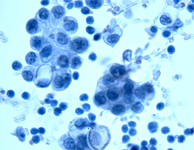
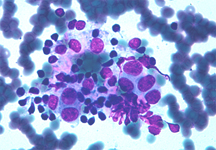
Melanoma
Dispersed cell population of cells with large vacuolated cytoplasm and evident nucleoli. Note cytoplasmic nuclear inclusion. Cells in a cell block are S100 positive.
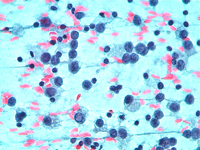
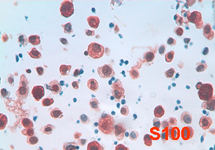
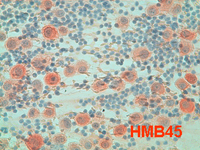
Melanoma
Isolated melanoma cells, intermingled with lymphocytes. Cells show dense large vacuolated cytoplasm, eccentrical atypical nuclei and evident nucleoli and are HMB45 positive.
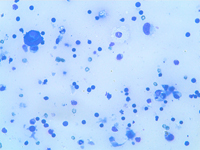
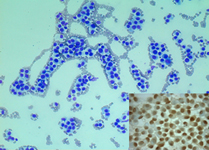
Papillary thyroid carcinoma
Papillary thyroid carcinoma may give precocious metastases to cervical lymph nodes. Metastases may be massive, focal or even cystic. Sometimes only few small groups of follicular cell are present; thyroglobulin immmunostain may confirm their thyrodal origin.
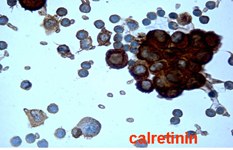
Mesothelioma
Infrequently mesothelioma may determine lymph-nodal metastases. Mesothelial cells show typical intercellular “windows”, positivity for cytokeratin, vimentin and calretinin and negativity for LCA with positive lymphocytes in the background.
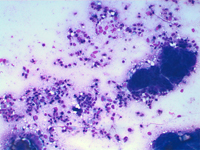
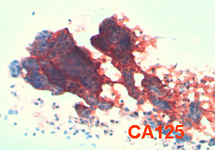
Ovary
Lymph nodal metastasis from ovary carcinoma showing thick, papillary epithelial structures and lymphoid cells in the background. Epithelial groups are CA125 positive.
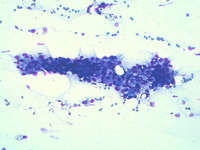
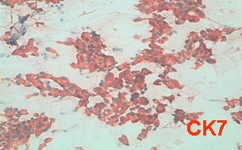
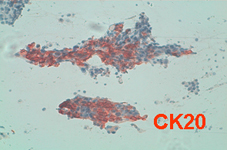
Bladder carcinoma
FNA of inguinal lymph node of a patient suffering from recidivant urinary bladder papillomas. Smears show an epithelial tumour, CK7 and CK20 positivity is consistent with an urothelial primary tumour.
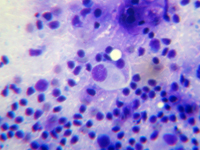
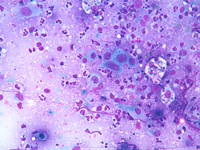
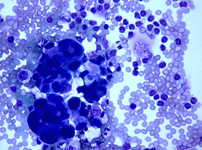
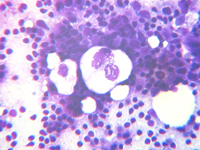
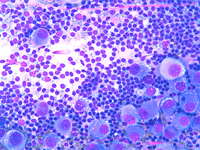
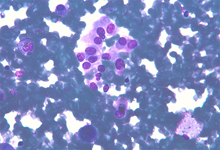
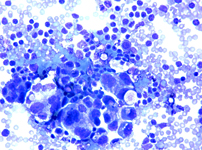
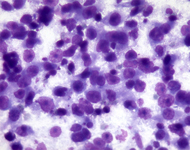
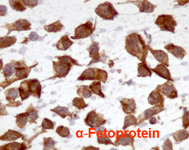
Disgerminoma (seminoma)
Dispersed, poorly differentiated large cells with evident nucleoli and fragile cytoplasm. The back ground is usually “dirty” with scattered lymphocytes intermingled. Cells are α-Fetoprotein positive.
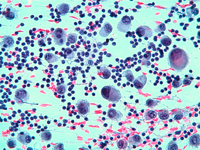
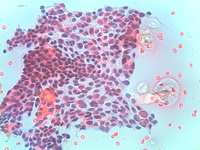
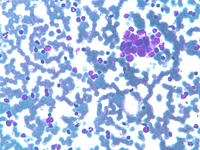
Breast carcinoma
Lymph nodal metastasis from breast carcinoma showing groups of ductal cells in a haematic background or intermingled with lymphocytes. Estrogens immunostain may be helpful to reveal the mammary origin.