Cervical Cytology
The Pap test : principles of collection and preparation of specimens. Laboratory organisation, screening and reporting cervical smears.
| The Pap Test |
| Collection of specimens |
| Guidelines on laboratory organisation, processing and screening |
| Terminology and reporting |
Development of the Pap test by Dr George Papanicolaou
Dr George Papanicolaou (1883-1962)
The role of the Pap test as a method of detecting preinvasive and early invasive cervical cancer
- The Papanicolaou smear test is used world wide as a screening test to detect preinvasive or early invasive cancer of the cervix
- The test involves removal of a sample of epithelial cells from the surface of the cervix using a spatula or other sampling device
- The cells are transferred onto a glass slide and sent to the cytology laboratory where they are stained and prepared for microscopic examination
- The initial microscopy is carried out by a cytotechnologist (primary screener) who is trained to detect abnormal cells among the many thousands of normal cells in the smear.
- Women who have abnormal smears are referred for further investigation and treatment.
- Detection of cervical cancer while it is still in the preinvasive stages has saved many lives.
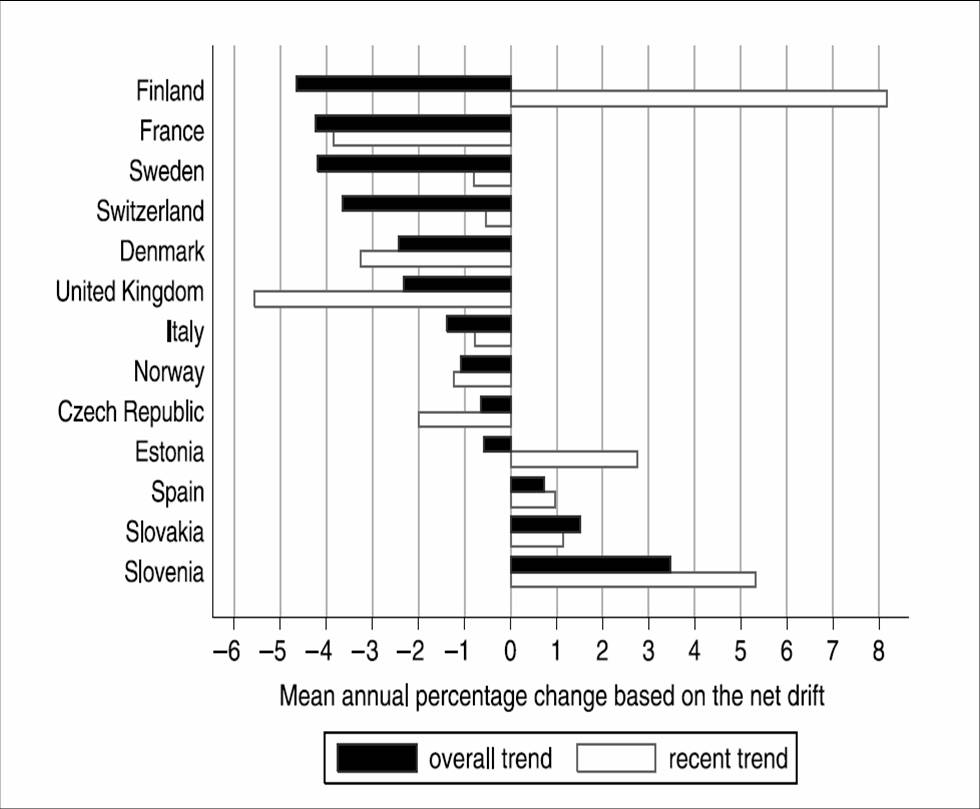
This diagram shows the trends in incidence of invasive cervical cancer in European countries between 1950 and 1990 and in the last decade (in the 1990s). It shows that increased incidence in those countries without a national screening programme (eg Estonia ,Slovenia) and decreasing incidence in countries with a national screening programme (eg UK, Denmark)
Aims of the Pap test
- The primary aim of the Pap test is to prevent the development of invasive cancer of the cervix by detecting precancerous lesions (Cervical Intraepithelial Neoplasia) in the uterine cervix. Conservative treatment of precancerous lesions by local ablation of the abnormal epithelium is a highly effective method of signficantly reducing the risk of invasive cervical cancer.
- The Pap test is also a sensitive tool for detecting early invasive cancer of the cervix. Women with early invasive cancer (FIGO Stage 1) are often unaware that they are harbouring the tumour as they are usually symptom free. Diagnosis and treatment of invasive cancer while it is still in the early stages of development signficantly improves the prognosis (chances of long term survival) of the patient.
- For these reason the Pap test is used primarily as a tool for screening healthy women for preinvasive cervical cancer (CIN) and early invasive cancer.
Other uses of the Pap test
- Although the most important use of the Pap test is as a tool for population screening tool to identify women at risk of cervical cancer , it can also be used as a diagnostic test for cervical cancer. It can be used to confirm the presence of invasive cancer in women with symptoms and/or signs suggestive of this disease.
- However, when it is used in this way , the results have to be interpreted with caution
- Studies have shown that the cervical smear may be negative even in the presence of an advanced invasive cervical cancer. This is because blood, inflammatory cells and necrotic debris from the cancer site frequently obscure the abnormal cells in the smear.
- Smear takers need to be alert to this fact and must employ other methods ie colposcopy and biopsy to ascertain the presence or absence of malignancy in a symptomatic patient with a negative Pap test.
- The Pap test is frequently used in the follow up of women who have been treated for CIN or invasive cancer. It is a sensitive method of detecting recurrence of disease in these patients.
- A range of specific infectious organisms can be diagnosed from the cervical smear. However the Pap test is not a sensitive method of detecting infection and this is not a primary use of the test.