Anaplastic carcinoma
It accounts for less than 5% of thyroid cancers and it is associated with a very poor prognosis. It presents clinically as a rapidly growing neck mass which usually has already infiltrated adjacent structures at the time of diagnosis. In about one-third of cases, anaplastic carcinoma is associated to a well-differentiated thyroid carcinoma (such as papillary or follicular carcinoma).
Cytologic diagnostic features
- mostly single cells
- marked nuclear pleomorphism
- irregular nuclear membrane, pseudoinclusions, large nucleoli
- large, epithelioid or spindle-shaped cells
- giant cells
Different patterns can be observed and the cytologic appearance is variable. The cells can be in large fragments, small clusters or as isolated cells. Often a tumor diathesis, including many necrotic cells, is noted. The cells can also be spindle and sarcomatoid. Very large, pleomorphic and bizarre cells may be observed, together with multinucleated tumor giant cells. In some tumors the cells can show squamous differentiation.
Differential diagnosis
- metastatic carcinoma
- medullary carcinoma
- radiation changes
In case of doubt, immunocytochemistry is helpful to distinguish anaplastic from medullary carcinoma, which is calcitonin-positive. Most of pure anaplastic carcinomas are thyroglobulin-negative, so the differential diagnosis from a metastatic carcinoma rests on the patient`s clinical history.
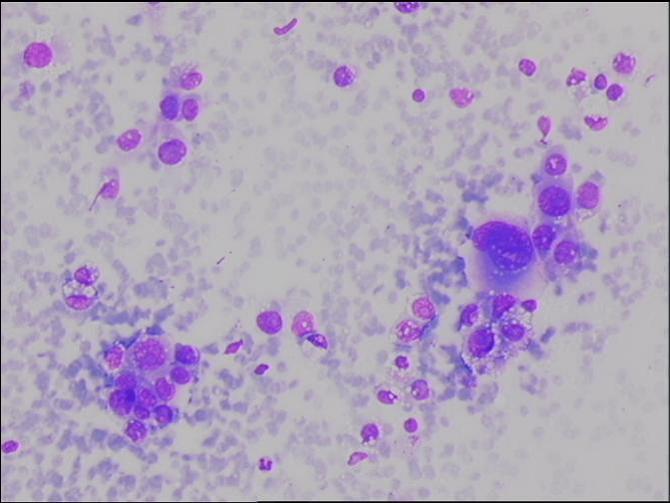
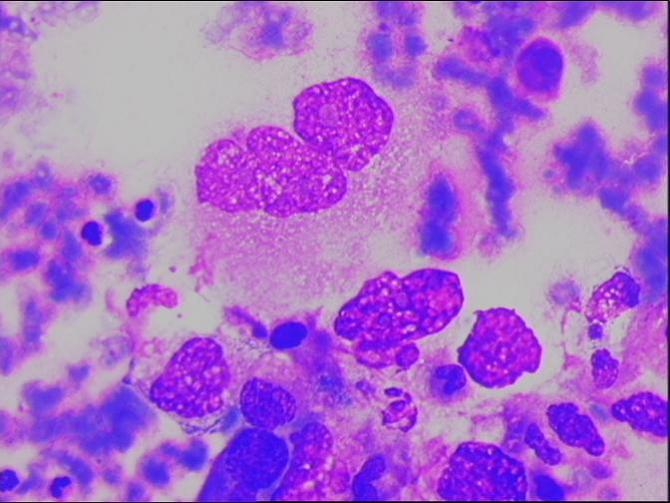
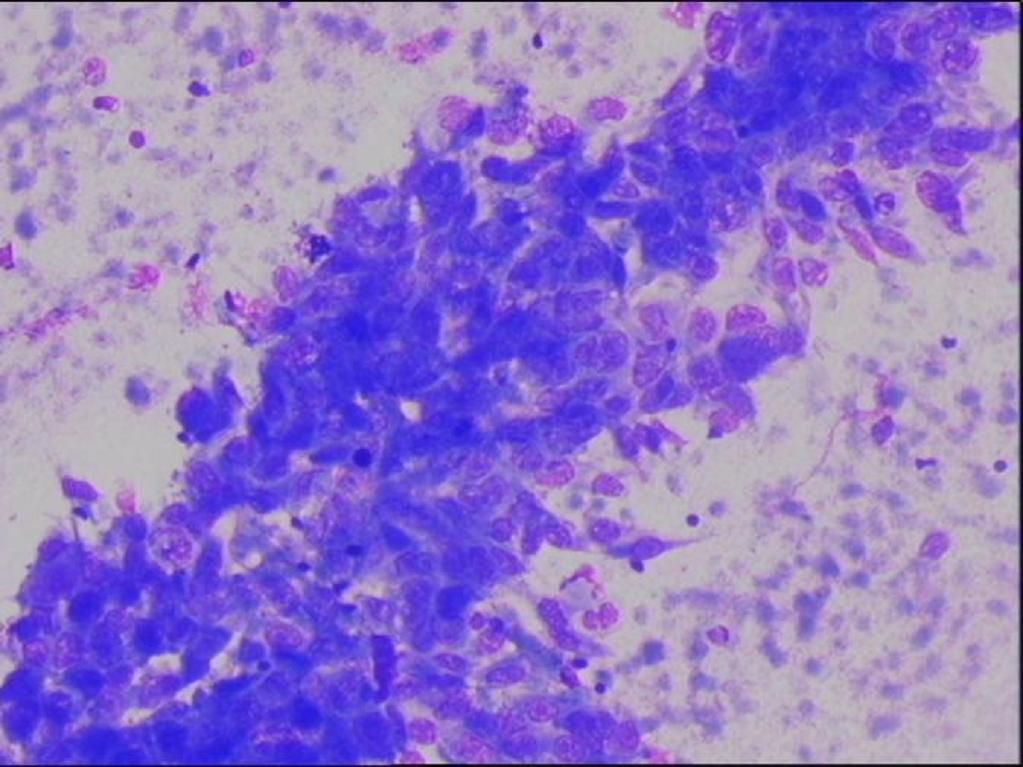
Cellular debris and large, very atypical (anaplastic) cells (MGG). Bizarre, multinucleated atypical cells (MGG) A crowded cluster of aytpical spindle cells from an anaplastic carcinoma (MGG)