Insular carcinoma
Some thyroid carcinomas have an intermediate grade of atypia between well-differentiated carcinomas and anaplastic carcinoma. These poorly differentiated carcinomas account for <5% of thyroid carcinomas. One distinctive form is insular carcinoma.
Cytologic diagnostic features
- high cellularity
- mostly single cells
- clusters, microfollicles
- monomorphous round nuclei
On hystologic preparations, malignant cells of insular carcinoma are arranged in nests ('insulae') or ribbons, surrounded by stroma. Cyologic smears are highly cellular, with numerous isolated tumor cells and clusters of overlapping cells. In some cases a minor population of large pleomorphic cells may be present as well. Cytoplasm is poorly defined, sometimes vacuolated. Nuclear grooves and pseudoinclusions may be observed in some cases. Colloid is scant.
When the characteristic nuclear changes are observed, they can suggest a papillary carcinoma, but the prominence of isolated cells is more typical of insular carcinoma. Focal nuclear pleomorphism may suggest an anaplastic carcinoma, but spindle and giant cells are uncommon. Insular carcinoma can resemble medullary carcinoma, but microfollicles with colloid can be helpful to the diagnosis and immunocytochemistry can be performed: insular carcinomas are thyroglobulin positive and calcitonin negative.
A correct diagnosis is rarely made by FNA; it can be made with certainty only after hystologic examination. Most specimens are diagnosed as follicular neoplasms or as metastatic carcinoma.
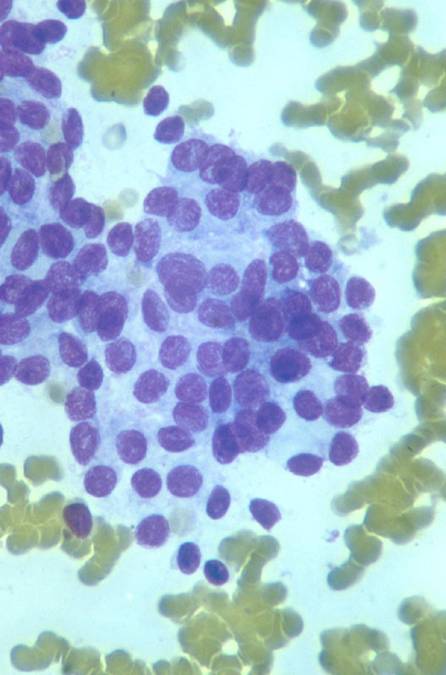
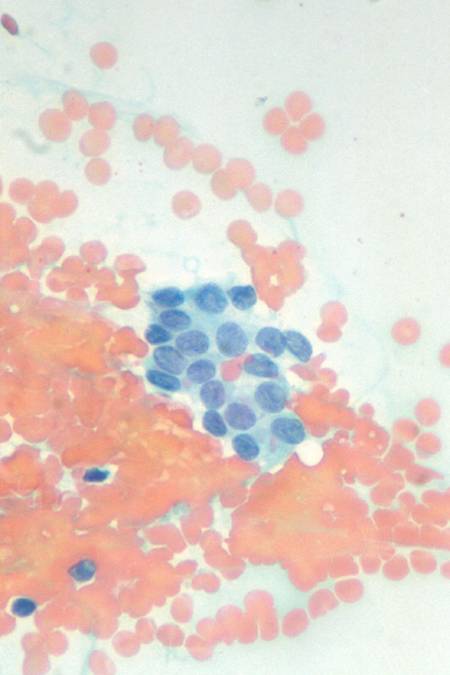
A crowded group of epithelial cells with coarse chromatin and higher N/C ratio (MGG). The nuclei have irregular outlines and chromatin pattern (Pap).