Papillary carcinoma
Papillary thyroid carcinoma (PTC) is the most common malignancy of the thyroid (>80% of thyroid cancers). It may occur at any age, but most patients are between 30 and 50 years old; most of them are female (F:M 3:1). It usually presents as a solitary, non-functioning ('cold') nodule, sometimes with cervical lymphadenopathy due to metastatization. The prognosis is usually very good
Many papillary carcinomas contain one of the chimeric ret/PTC oncogenes, resulting from rearrangements involving the ret oncogene on chromosome 10.Cytologic diagnostic features
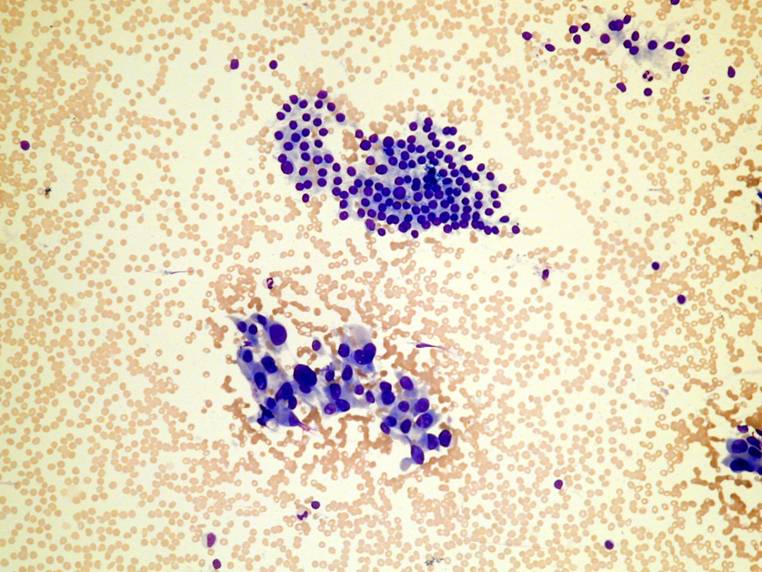
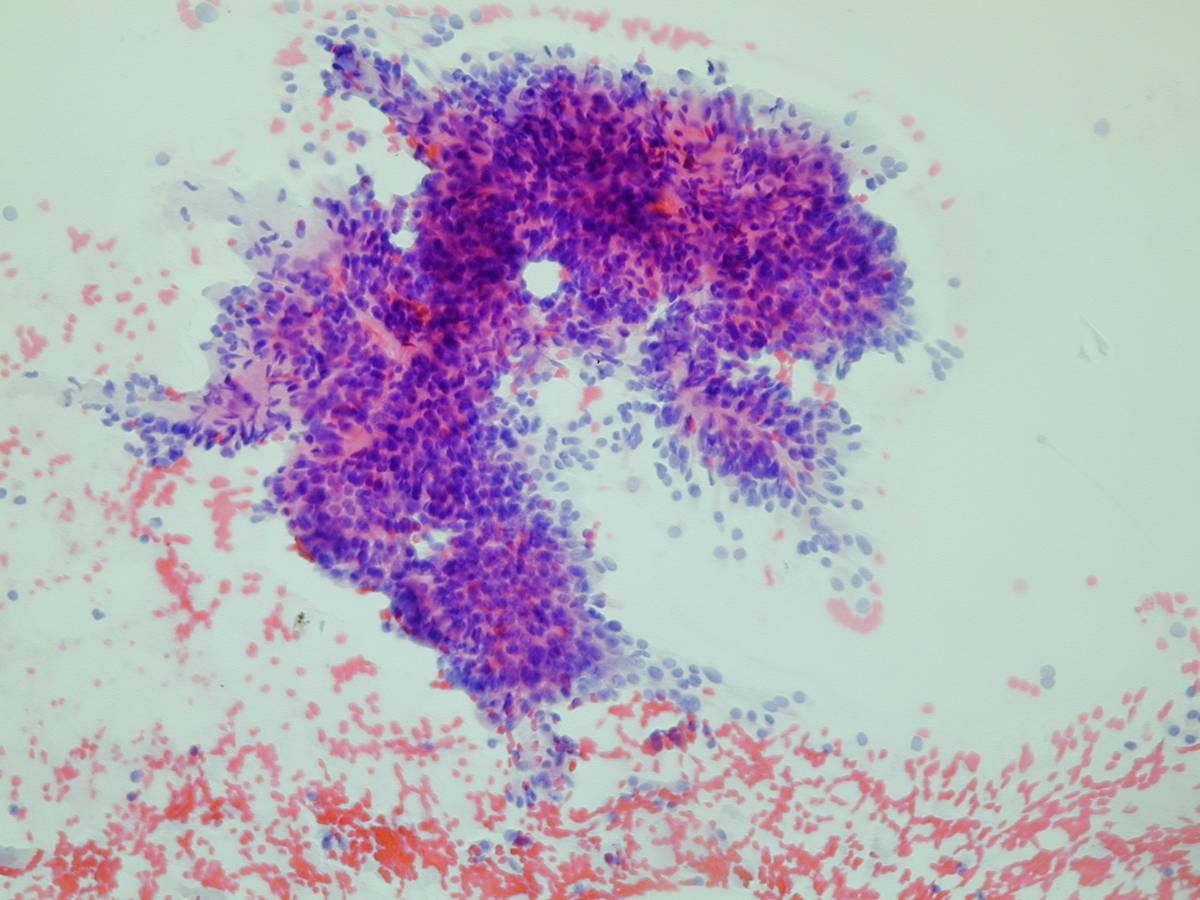
- papillae, sheets, microfollicles
- nuclear changes
- nuclear enlargement
- 'powdery' chromatin
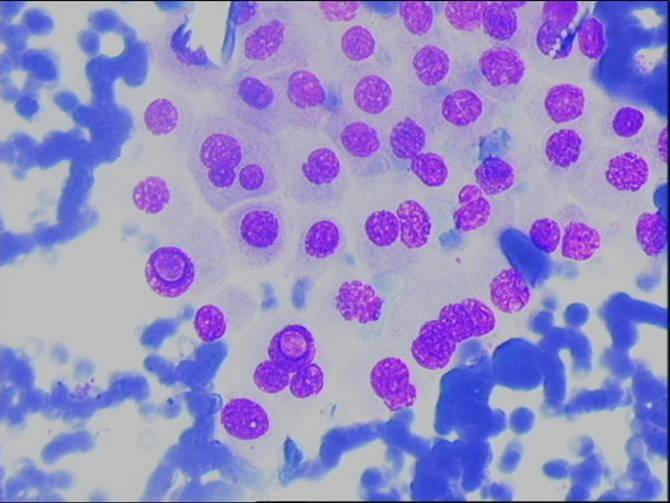
- nuclear pseudoinclusions and grooves
- nucleoli (small or large)
- irregular nuclear membrane
- nuclear crowding and molding
- variable cytoplasm (scant, squamoid, Hürthle-like, vacuolated)
- psammoma bodies
- histiocytes (multinucleated giant cells)
Typical architectural features are papillae (with neoplastic cells lining a fibrovascular core); microfollicles are observed in the follicular variant of papillary carcinoma. The diffuse sclerosis variant can be hard to recognize. Mixed variants may be observed as well.
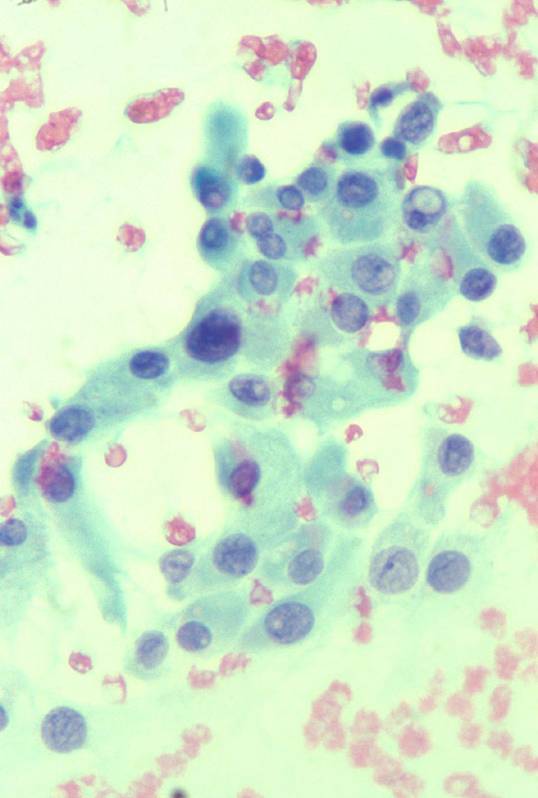
The recognition of papillary formations is very helpful but not necessary as it is lacking in the follicular variant of papillary carcinoma. The diagnosis does not rest on architectural features, but on the characteristic nuclear changes: longitudinal grooves, nuclear pseudoinclusions, a pale, 'powdery' chromatin pattern. A characteristic feature of papillary carcinoma is increased cytoplasmic density, which is present in most cases (66%-100%) giving rise to the so-called 'squamoid cells'.
Colloid is present and sometimes abundant. It can have an abnormal viscosity ('bubble gum' colloid) and may take the shape of long strands or dense blobs. Psammoma bodies (which are laminated calcifications) are a helpful diagnostic feature, but are not frequently observed on cytologic smears. The presence of cystic degeneration, usually with several macrophages in the smear, could lead to a false-negative diagnosis: follicular cells are always required to consider a smear as adequate.The aggressive variants of papillary carcinoma may be recognised by large cell size, numerous intranuclear cytoplasmic invaginations, marked nuclear pleomorphism, coarse chromatin, or abundant dense, granular cytoplasm.
Two rare variants of papillary carcinoma have distinctive diagnostic features. The tall cell (or pink cell) variant is characterized by cells with abundant pink cytoplasm, with the nuclear features of papillary carcinoma. Because of the 'tall', often granular cytoplasm, they may resemble Hürthle cells. The prognosis is worse than that of the classical variant of papillary carcinoma. The columnar cell variant is composed of crowded tall, columnar cells, with the nuclear features of papillary carcinoma.Differential diagnosis
- benign thyroid nodule (e.g. nodular goiter)
- follicular neoplasm
- hyalinizing trabecular adenoma
- radiation changes
Although grooved nuclei are usually present, they are sparse in as many as 25% of cases and absent in up to 10% of cases. Nuclear grooves may be present in other benign thyroid diseases such as thyroiditis and goiter. Nuclear pseudoinclusions are instead the most important qualifiers of papillary carcinoma and should always be present. Since they are surrounded by nuclear membrane, they have a very sharp margin, which is often outlined by a rim of condensed chromatin. Although pseudoinclusions may be present in other primary (Hürthle cell tumours, medullary carcinoma, insular carcinoma) or secondary tumours (melanoma) they are exceptional in benign diseases of the thyroid. In FNA biopsy of the thyroid, therefore, these inclusions represent a strong argument for a cancer diagnosis, usually papillary carcinoma, when combined with other diagnostic features. The follicular variant of papillary carcinoma can be difficult to distinguish from a follicular lesion; the chromatin pattern can be helpful. The hyalinizing trabecular adenoma can have the nuclear features of papillary carcinoma, and most case are diagnosed as suspicious or positive for papillary carcinoma by FNA. Only histologic examination is able to make a differential diagnosis, showing encapsulation, trabecular architecture and marked stromal hyalinization. Some of the nuclear features (grooves, pseudoinclusions) of papillary carcinoma can be occasionally seen in benign nodules after iodine administration, but in this case nuclei are usually hyperchromatic and variable in size.
FNA is highly accurate in diagnosis of PTC and indeed because of the relative incidence of this type of thyroid tumour it explains the very high sensitivity of FNA for malignancy.
Cytologic grading of papillary carcinoma
Score 1 Score 2 Score 3 Cell size = pmn = 2 pmn = 3 pmn pseudoincl. x 5 hpf < 5 5-10 > 10 nuclear pleomorphism mild moderate severe chromatin fine granular coarse
- Low grade (score <= 8) usually classic variant at histology
- Intermediate (score 9-11)
- High grade (score >11) usually aggressive variants at histology
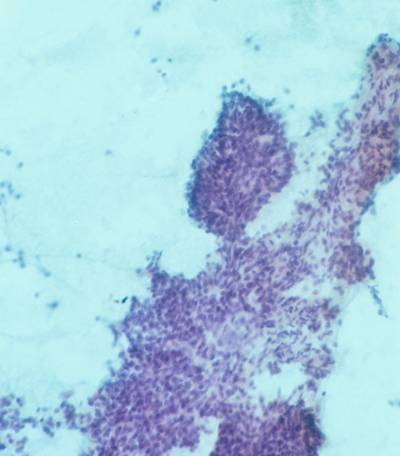
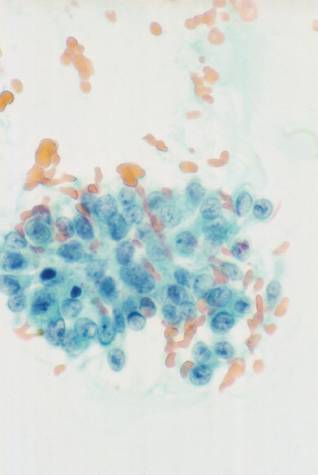
A small cluster of cells with the nuclear feature of PTC. A group of 'squamoid' cells with the nuclear features of PTC.
A large fragment from a PTC. A group of blander cells from a PTC.