| The female genital tract |
| The Uterus and cervix |
| The vagina |
| Evaluation for hormonal status |
The vagina
The vagina is a fibromuscular canal about 7 cm long which extends from the vestibule to the cervix. Thus it communicates with the body of the uterus via the endocervical above and the exterior below. It is capable of marked distension and elongation during parturition. The vagina forms a cuff around the lower two thirds of the cervix to form the anterior, posterior, and lateral vaginal fornices.
The vagina is lined by stratified non keratinising squamous epithelium which varies in thickness and structure throughout life. In the prepubertal female and the post menopausal woman the epithelium is thin and comprised of a basal layer of cells and several layers of parabasal cells. This thin atrophic epithelium is vulnerable to infection and frequently shows the degenerative and inflammatory changes of non specific vaginitis.
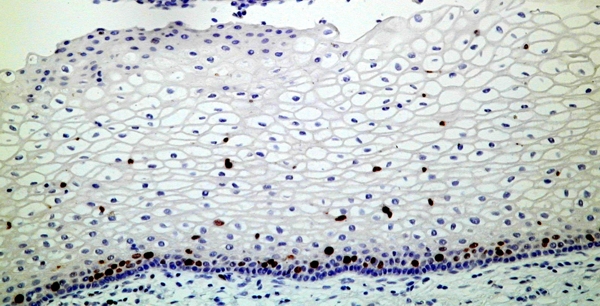
During reproductive life the vaginal epithelium reflects the hormonal changes of the menstrual cycle and reflect increased mitotic activity of the basal layers. Under the influence of oestrogen in the proliferative phase of the cycle, the whole epithelium thickens and is multilayered. The mature epithelial cells at the surface are large, flattened and angular and have dense small pyknotic nuclei (< 4 u). During the secretory phase of the cycle, the intermediate layers thicken and the cells become stuffed with glycogen. Breakdown of glycogen by lactobacilli which are commensal in the vagina produces an acid pH in the vagina which deters infection by bacteria and fungal infections such as candida albicans.Hormonal cytology: The vaginal squamous epithelium is a much more sensitive register of hormonal change than is the squamous epithelium of the cervix. As a result, cytological smears of the vaginal wall can be a useful guide to the hormonal status of the patient. The changes in the smear pattern throughout the menstrual cycle can be used as a rough guide to ovulation. A typical post partum pattern and post menopausal pattern can also be recognised. However, there are certain caveats which limit the usefulness of hormonal cytology in clinical practice.
The place of hormonal cytology in clinical practice
- A gentle scrape should be taken from the upper third of the vaginal wall as this portion of the vagina is derived embryonically from the Mullerian duct and hence is the most hormone sensitive region of the vagina. Even so , the characteristic smear patterns only develop several days after exposure to oestrogen or progesterone
- Although the vaginal epithelium is most sensitive to oestrogen and progesterone, the epithelium also responds to other hormones such as androgens corticosteroids and thyroxine. It also responds to digitalis, anticancer therapy, oral contraceptives and hormone replacement therapy. Thus a full medical history as well as a menstrual history and exposure to exogenous oestrogens e.g. in face cream should be taken before issuing hormone cytology report.
- Chronic inflammation and infection may result in proliferation of the epithelium. For example, Trichomonas vaginalis infection is typically associated with a mature proliferative pattern. Hyperkeratosis may be noted if there is prolapse of the uterine cervix into the vagina. Thus smears which show evidence of inflammation, radiotherapy changes, hyperkeratosis or specific infection are unsuitable for hormonal evaluation
- Cervical smears should not be used for hormonal estimates as metaplastic changes and the effects of infection can be misleading.
- In the past, claims were made that hormone cytology can be used to predict spontaneous abortion or term pregnancy but these claims have not been substantiated and the reliable diagnosis of these conditions depend on biochemical methods or imaging. Sequential smears need to be taken if hormone cytology is used to determine ovulation.
The mature squamous epithelium of the vagina consisted of 18-20 layers of epithelial cells which can conveniently be divided into three zones.
- The superficial zone (synonym surface zone)
- The mid zone (synonyms the parabasal zone or intermediate zone)
- The basal layer (germinal layer, basal and suprabasal layers)
Under the influence of oestrogen, the vaginal squamous epithelium proliferates to its full thickness and the surface layers are composed of large (30-40um diameter) angular squames with structureless pyknotic nuclei.2-3um in diameter .These predominate in smears taken mid cycle.
Under the influence of progesterone the epithelium thickens but proliferation is confined to the cells of the mid zone. Smears are composed of large glycogen filled cells boat shaped cells (20-30 um diameter) with abundant basophilic cytoplasm; their nuclei of the cells are vesicular and have a delicate chromatin structure. These cells are termed navicular cells and they predominate in the second half of the cycle. When progesterone secretion is prolonged (as in pregnancy) the navicular cells have greatly thickened borders and form dense clusters in the smear. Lactobacilli catabolise the cells for their glycogen content and bare nuclei and cytoplasmic fragments form the background to the smear.
In the absence of hormone secretion e.g. puberty, post partum or after the menopause, the vaginal epithelium thins to only a few layers. After the menopause smears reflect the vaginal atrophy and are composed of small (10um) rounded fragile parabasal cells. The cells may be present as discrete cells or in large sheets. They usually have large open nuclei occupying about 1/3 of the area of the cell and delicate basophilic cytoplasm .The nuclei may be pyknotic or exhibit karyorrhexis and evidence of infection is common. In lactational or postpartum smears the parabasal cells are typically glycogenated. A similar pattern may be found when virilising ovarian tumours are present or exogenous testosterone is given as part of a treatment regime for lichen sclerosis.
Interestingly, a vaginal smear from a newborn female may exhibit some epithelial proliferation reflecting the trancplacental transfer of maternal hormones in utero but the changes are temporary and an atrophic pattern supervenes.