| The female genital tract |
| The Uterus and cervix |
| The vagina |
| Evaluation for hormonal status |
The uterus
The uterus is a pear shaped organ located between the bladder and the rectum. In the non pregnant female it is about 3 inches (7 cm) in length and is normally in an anteverted position. The upper portion of the uterus is the fundus whereas the larger central portion of the uterus is known as the corpus uteri or body of the uterus. The narrow lower portion of the uterus is the cervix uteri (which means neck of the uterus) which in turn open into the vagina. The fundus and body of the uterus have thick muscular walls (the myometrium) which thicken in pregnancy and a specialised mucosal lining (the endometrium) which is capable of supporting the developing fetus.
The endometrial lining of the uterine cavity consists of pseudostratified columnar ciliated epithelium and is supported by a cellular stroma containing numerous tubular glands. Under the influence of oestrogen and progesterone secreted by the ovarian follicles, the endometrium undergoes regular cyclical changes which prepare the uterus for the reception of the fertilised ovum. Successful implantation can only occur if the endometrium provides the early embryo with an abundant supply on nutrients.
The cycle of changes in the endometrium proceeds through two distinct phases: the proliferative phase and the secretory phase.
Summary of one female menstrual cycle: A. Ovatian cycle; maturation of follicle and development of corpus luteum. B. Anterior pituitary cycle; LH and FSH levels. C. Uterine cycle; menstrual, proliferative and secretory phases. D. Ovarian hormone cycle' oestrogen and progesterone levels. (Ross and Wilson: Anatomy and Physiology in health and illness; figure 19.10)
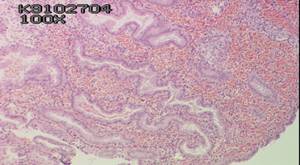
The proliferative phase: The proliferative phase is initiated and sustained until ovulation by the increasing production of oestrogen by the developing ovarian follicles. It is characterised by proliferation of the endometrial stroma which becomes thicker and more vascular. The simple tubular glands proliferate to form numerous glands which start to secrete mucous. (INSERT HISTOLOGY SECTION HERE SHOWING PROLIFERATIVE PHASE ENDOMETRIUM)
The secretory phase: is characterised by increasing tortuosity of the glands under the influence of progesterone secreted by the corpus luteum. The glands produce a copious glycogen rich secretion which is an important source of nutrition for the fertilised ovum.
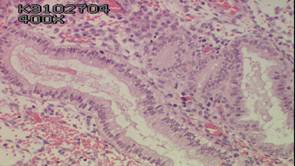
Endometrium in the early secretory phase. Note sub nuclear vacuoles and the slight tortuosity of the gland
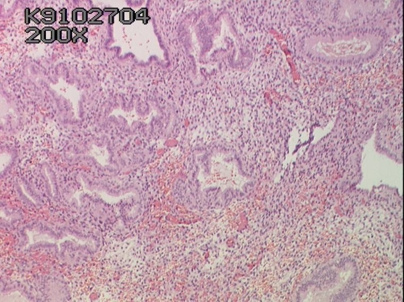
Mid secretory phase of the cycle the sub nuclear vacuoles move to the super nuclear position and secrete their contents into the glands which become increasingly dilated and tortuous. Note oedatous stroma due to increased blood flow.
Late secretory endometrium. The stroma consists largely of sheets of pre decidual cells infiltrated by polymorphs and lymphocytes. These increase in number as the endometrium undergoes menstrual changes characterised by necrosis glandular collapse and haemorrhage.
Menstruation: In the absence of implantation of a fertilised ovum, the corpus luteum degenerates and oestrogen and progesterone secretion ceases. Constriction of the spiral arteries of the endometrium results in ischaemia and collapse of the endometrial glands and the onset of menstruation. By the third or fourth day of menstruation, most of the endometrial lining has been shed and proliferation of the basal layers of the endometrium starts again.
The Pregnant Uterus:
When the ovum is shed from the ovary at ovulation, it is wafted into the fimbriated end of the Fallopian tube. Fertilisation usually takes place at this site and the fertilised egg is conveyed along the tube to the endometrial cavity. At about the 7 day after fertilisation the ovum attempts to implant in the uterine wall. If implantation is successful the corpus luteum enlarges and continues to secrete oestrogen and progesterone so that the glycogen rich endometrium does not involute. At about 12 days implantation is complete. Under the influence of progesterone the stromal cells of the endometrium undergoes decidual change and eventually dominate the endometrium,The stromal cells are large with prominent pale staining round nuclei and bulky cytoplasm. Ultimately the decidua basalis (which is the decidual layer immediately beneath the implantation site), the chorionic villi from the fetus and the intervillous spaces fuse to form the placenta. .
The post menopausal uterus
After the menopause the cyclical production of oestrogen and progesterone by the ovaries ceases and the whole genital tract undergoes atrophic changes. The endometrium is thin and consists of scanty stroma and sparse, inactive glands.
The uterine cervix
(For a more detailed account of the anatomy, physiology and histology of the cervix please go to next section)The cervix is the narrow inferior segment of the uterus which projects into the vaginal vault. It is a fibromuscular organ lined by mucous membrane and measures 3 cm in length and 2.5cm in diameter. In the adult female, it is angled downwards and backwards. In the nulliparous female it is barrel shaped but it changes shape in pregnancy and the menopause. The cervix is continuous above with the body of the uterus and is continuous below with the vagina .About half the length of the cervix (the portio vaginalis) extends into the vagina. This portion is covered with stratified squamous epithelium which is continuous with the vaginal squamous epithelium. The cervix is traversed by the endocervical canal which is lined by glandular epithelium.