Cervical Cytology
Glandular lesions and management of women with abnormal smears.
| Biological relationship of adenocarcinoma and adenocarcinoma in situ (AIS) |
| Cytology of adenocarcinoma |
| Atypical glandular cells |
| Recommendations for management |
Morphological and biological characteristics of cervical adenocarcinoma and adenocarcinoma in situ
- Adenocarcinomas constitute 5 - 10 % of all carcinomas arising in the cervix.
- Several histological types are recognised including endocervical adenocarcinoma, endometrial adenocarcinoma and clear cell carcinoma. The endocervical type is most commonly found and most readily recognised in cervical smears. However, it is not uncommon for more than one type of adenocarcinoma to be present in a single tumour
- The frequent coexistence of cervical adenocarcinoma with squamous carcinoma suggest that they have a common aetiology and pathogenesis. HPVDNA is found in both and both are associated with the same risk factors.
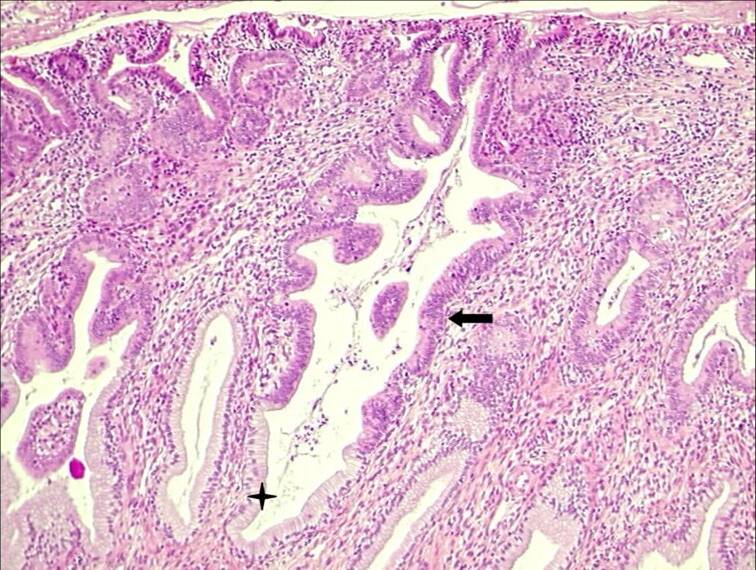
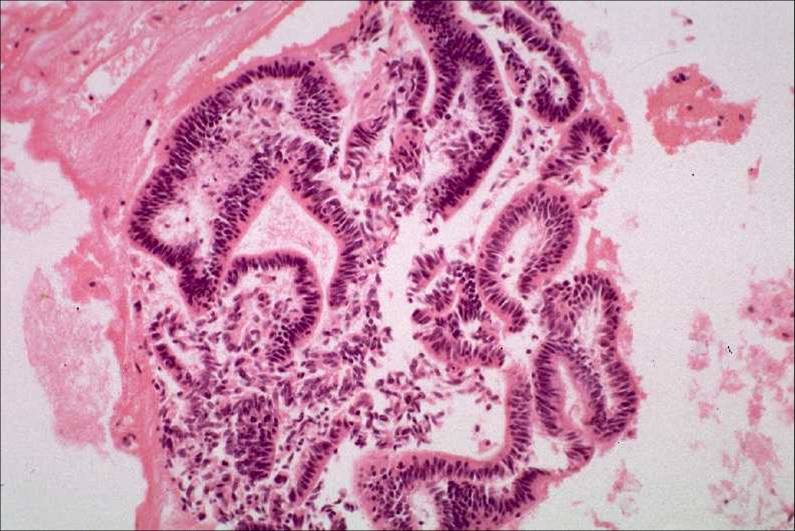
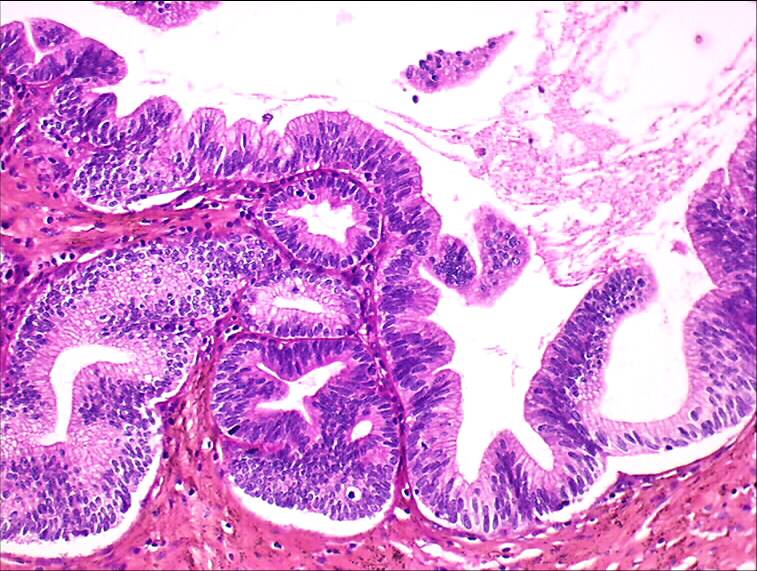
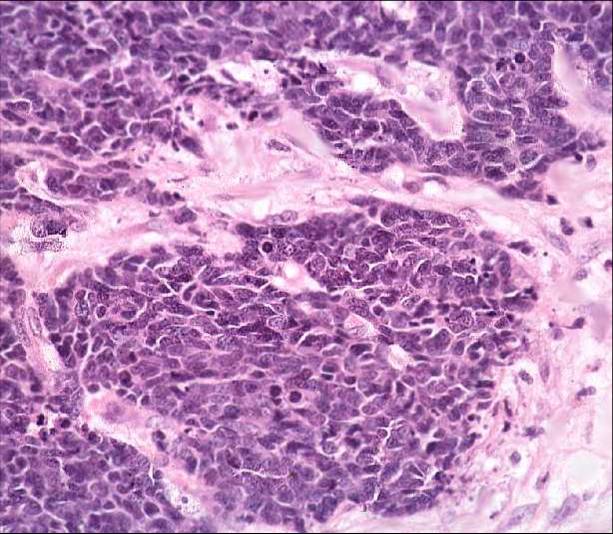
- Endocervical adenocarcinoma may be polypoid or ulcerative. The tumour is composed of branched and budding glands lined by mucin producing neoplastic cells which resemble the glandular cells lining the endocervical canal. Three grades of adenocarcinoma are recognised well– differentiated, moderately differentiated and poorly differentiated according to how closely the morphology of the tumour resembles that of the endocervix.
- Endocervical adenocarcinoma in situ is considered to be the glandular counterpart of cervical intraepithelial neoplasia and a precursor of invasive adenocarcinoma.
- Although the invasive and the in situ forms of endocervical adenocarcinoma can be recognised in histological section, a reliable distinction cannot be made from the appearance of the cells in the cervical smear.
Histology of adenocarcinoma of cervix
Endocervical adenocarcinoma (well differentiated)