| Anatomy and histology of the pancreas |
| Fine needle aspiration (FNA) and other sampling methods |
| Reporting terminology |
| Normal cells |
| Pancreatitis |
| Pancreatic cysts |
| Solid tumors |
| Biliary tract cytology |
Pancreatic pseudocysts
Pancreatic pseudocysts occur in the setting of acute pancreatitis, resulting from autodigestion of the parenchyma. They account for the vast majority of pancreatic cystic lesions (75-90%). Pseudocysts can be rarely associated with trauma or pancreatic surgery.
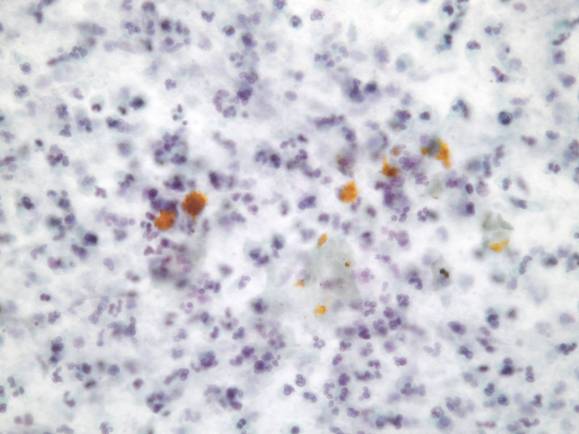
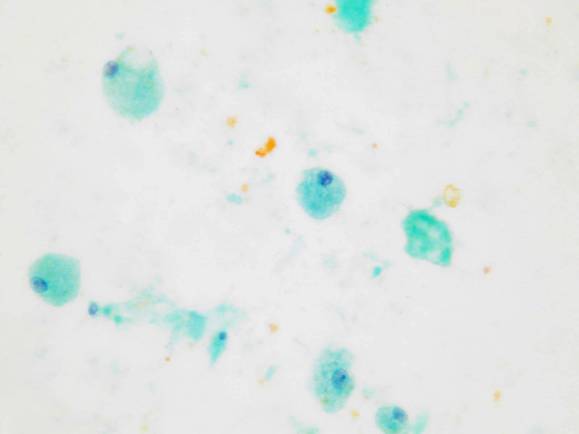
By definition, a pseudocyst lacks an epithelial lining. It is an unilocular thick-walled lesion, composed of an inflammatory fibrous capsule surrounding a region of necrosis. A communication with a pancreatic duct may be present. FNA yields abundant dark brown, turbid fluid and smears are composed of granular necrotic debris, blood, neutrophils and macrophages (also hemosiderin-laden macrophages). Aspirates may also contain pancreatic cells, fibroblasts and mesothelial cells. The diagnosis of pseudocyst on cytology should be considered one of exclusion.
- Cyst debris with blood, proteinaceous material and sometimes bile
- Variable inflammation
- No cyst lining epithelium (beware of contamination, mucin and epithelium)
Other non-neoplastic cysts
Other non-neoplastic cysts include retention cysts, cysts secondary to infections and congenital cysts; they are very rare and the diagnosis requires correlation with clinical findings.