| Anatomy and histology of the pancreas |
| Fine needle aspiration (FNA) and other sampling methods |
| Reporting terminology |
| Normal cells |
| Pancreatitis |
| Pancreatic cysts |
| Solid tumors |
| Biliary tract cytology |
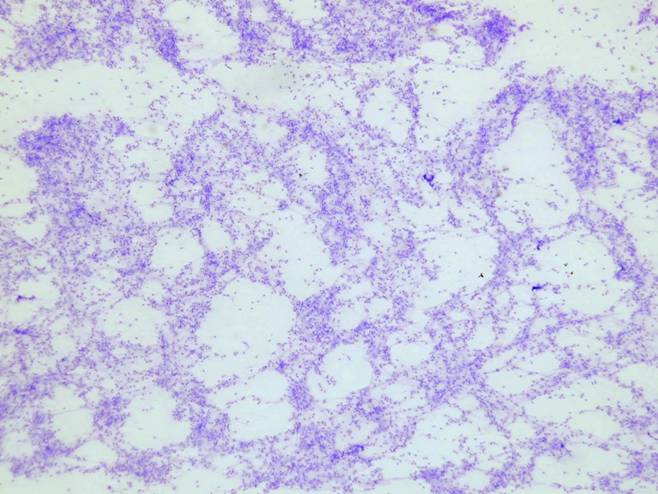
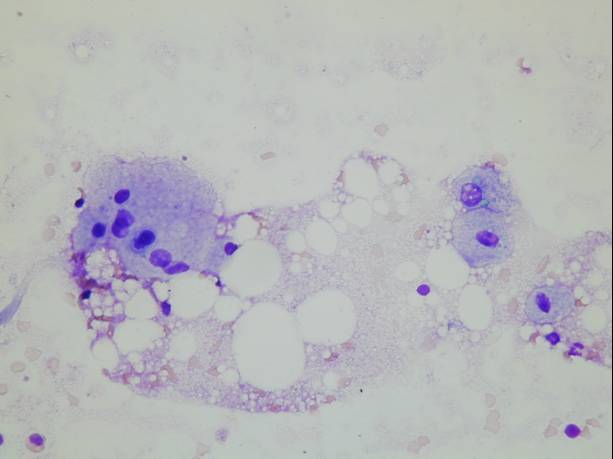
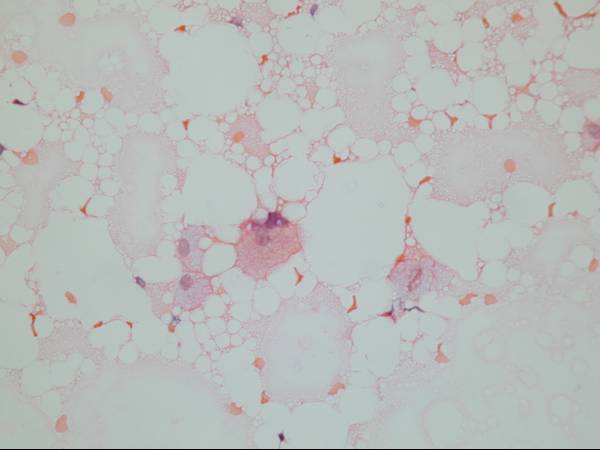
Acute pancreatitis
Acute pancreatitis results from the enzymatic autodestruction of the parenchyma and the accompanying acute inflammatory response. It is most commonly associated with biliary tract disease or alcoholism. The diagnosis rests on clinical findings and laboratory evidence, and the radiologic appearance is usually not suggestive of a mass lesion. For this reason, it is seldom aspirated. Aspirates are composed of a background of necrotic debris with degenerating cells, foamy histiocytes, fat necrosis, calcifications and acute inflammation.
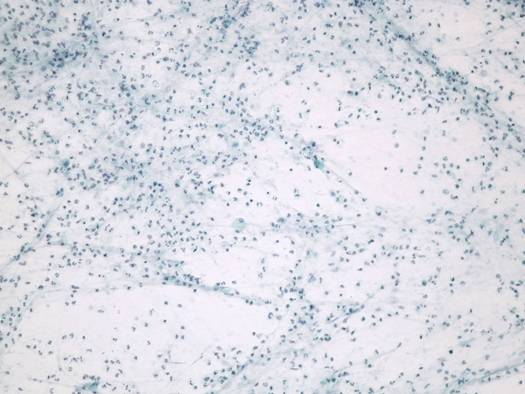
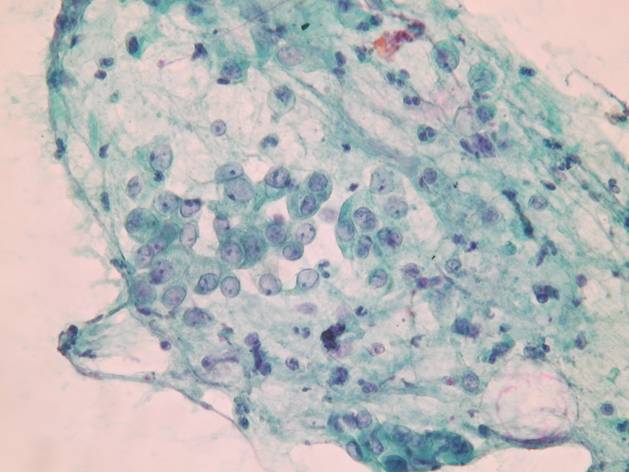
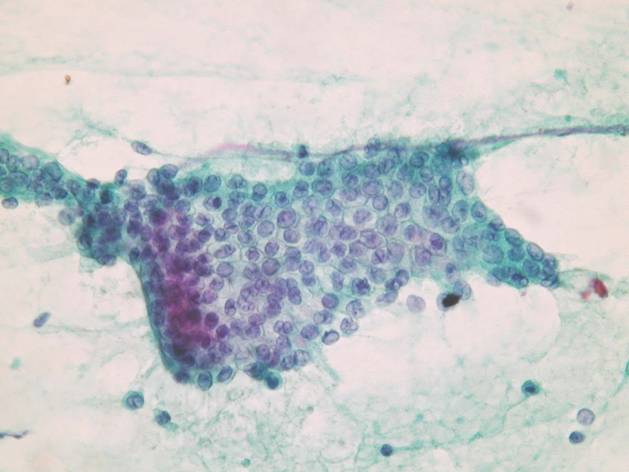
Chronic pancreatitis
Chronic pancreatitis may be difficult to distinguish radiologically from a neoplastic process. The cytologic appearance varies depending on the stage of the disease. Earlier stages are more cellular and contain a mixed lymphohistiocytic infiltrate. Later stages are sparsely cellular with less chronic inflammation and may show a relative predominance of islet cells due to atrophy of the acinar epithelium and the extensive fibrosis of the pancreatic parenchyma.
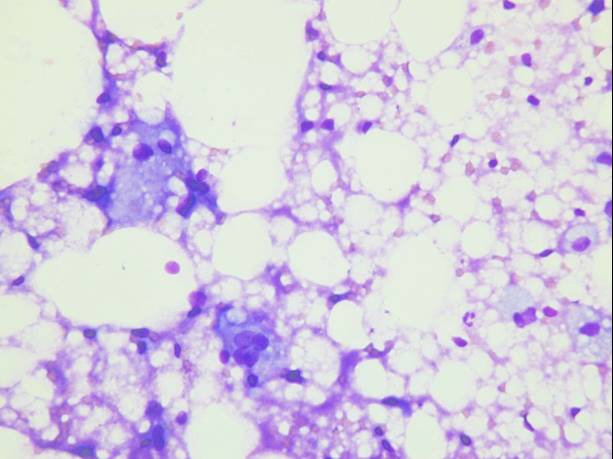
Early stages of chronic active pancreatitis
- Both ductal and acinar cells
- Background inflammation
- Granulation tissue
- Fat necrosis
Late chronic pancreatitis
- Mostly ductal cells
- Few to no acinar cells
- Some islet cells
- Monolayered sheets
- Cohesive, few single cells
- Maintained polarity
- Minimal nuclear overlapping
- Mild anisonucleosis
- Smooth nuclear membranes
- Rare/normal mitoses
- No coagulative necrosis
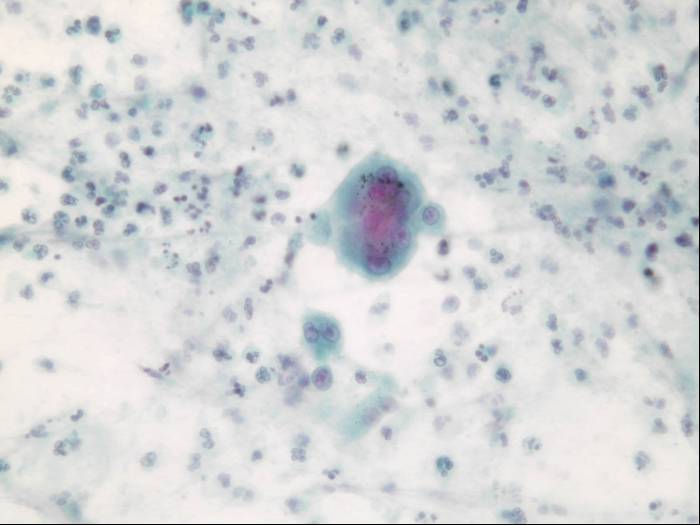
In both acute and chronic pancreatitis, the ductal epithelium may show marked reactive atypia which can be very hard to distinguish from an adenocarcinoma. Mitoses, prominent nucleoli, hypercromasia and nuclear enlargement are present both in reactive conditions and ductal adenocarcinoma.
Reactive ductal atypia - cytologic diagnostic features
- Low cellularity
- Flat, cohesive sheets
- Uniformly spaced, round to oval nuclei
- Rare intact single atypical cells