TRAINING OF CYTOTECHNOLOGISTS IN EUROPE
A DATABASE PREPARED BY
THE EUROPEAN ADVISORY COMMITTEE ON CYTOLOGY FOR THE EUROCYTOLOGY WEBSITE PROJECT
Tasks of the EACC
To obtain information from each EFCS member country by means of a questionnaire to prepare a database of the status of cytology training and to identify needs of cytology training.
Method
Twenty six cytotechnologists from 22 countries were identified and invited to participate in the study. Contact was by e mail and the contacts were asked to complete the questionnaire below.
Once the questionnaires had been returned the results were analysed and collatedQuestionaire
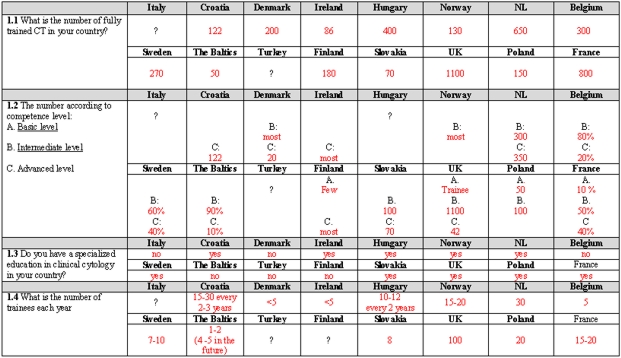
1.1 What is the approximate number of fully trained Cytotechnologists in your country?
1.2 The number according to competence level:
A. Basic level (cannot report negative or
unsatisfactory specimens)B. Intermediate level (can report negative and unsatisfactory specimens, can undertake rescreening and offer a differential diagnosis on abnormal specimens)
C. Advanced level (can report normal and
abnormal specimens)1.3 What is the approximate number of persons training to be Cytotechnologists (trainees) each year?
Please elaborate on your requirements:
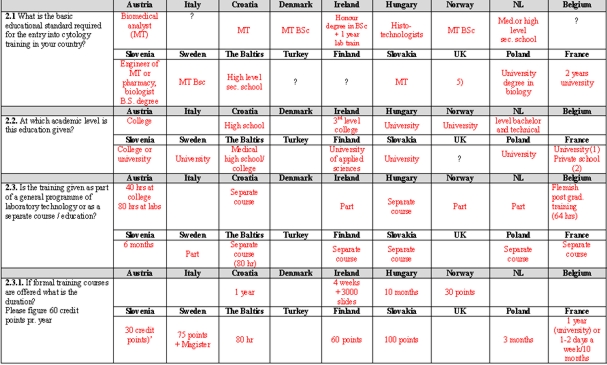
2.1 What is the basic educational standard required for the entry into cytology training in your country?
(eg. technician, medical technologist or other)2.2. At which academic level is this education given?
(eg. high school, college, university or other)2.3. Is the training given as part of a general programme of laboratory technology or as a separate course / education?
2.3.1. If formal training courses are offered what is the duration? Please figure 60 credit
points pr. year2.3.2. Which subjects are included in the curriculum?
(Please specify)2.4. Is the training given by instructors at the workplace? (Other; please specify)
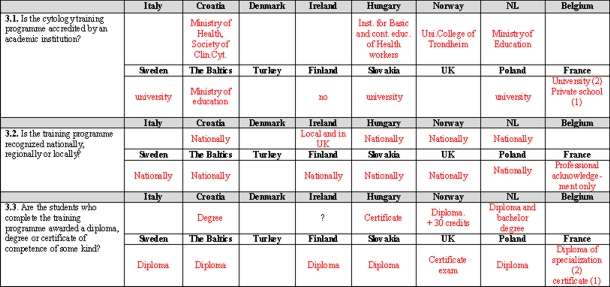
3.1. Is the cytology training programme accredited by an academic institution? (university, college or other; please specify)
3.2. Is the training programme recognized nationally, regionally or locally?
3.3. Are the students who complete the training programme awarded a diploma, degree or certificate of competence of some kind?
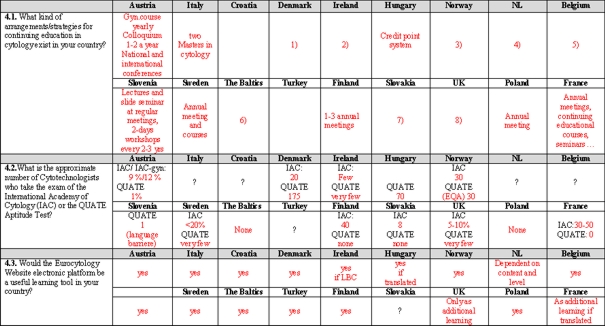
4.1. What kind of arrangements/strategies for continuing education in cytology exist in your country?
4.2.What is the approximate number of Cytotechnologists who take the exam of the International Academy of Cytology (IAC) or the QUATE Aptitude Test?
4.3. Would the Eurocytology Website electronic platform be a useful learning tool in your country?
Thank you!
Please return the questionnaire to Dorthe Ejersbo as soon as possible.
Dorthe Ejersbo
EACC Secretary
Department of Clincal Pathology
Winsløwparken 15
DK-5000 Odense C
DenmarkE-mail: dorthe.ejersbo@ouh.fyns-amt.dk
Tel: +45 65 41 18 29Results
Twenty six people from twenty two countries were contacted by e-mail. Responses were received from 17 countries. There was no response from Slovenia, Czech Republic, Spain, Germany and Albania. Latvia replied on behalf of the baltic community.
Contact persons
Results sheet
- Cytology screeners – high school education and the in-house two year training programme in gynaecological cytology.
- Biomedical Scientists – degree level entry (BSc in Biomedical Sciences) and then specialist training in both gynae and diagnostic cytology in-house
Summary of findings
The questionnaire was circulated initially to the named contacts in 23 countries .The first time there were responsed from 14 countries. The questionnaire and responses was circulated again to all contacts in 23 countries for comment. This encouraged three more countries to reply . Thus 17 countries responded in all .
The accuracy of the responses is limited by the competency of the individual respondents in the English language and the wide diversity of training and education in cytotechnology in Europe .The database shows that the number of cytotechnologists in training exceeds 4000. The level of training varies considerably between the different countries from high school level to BSc or MSc level. Eleven countries report that they have cytotechnologists rworking on the advanced level C (can report normal and abnormal smears .) This probably reflects the difference in reporting practice in the individual laboratories /countries more than the actual level of eduction or training. The respondents seem to have access to the internet and would see the Eurcytology website as a useful learning tool.
Professor Reidun Mecsei (Norway)
Chairman, European Advisory Committee for Cytology September 30, 2006Ms Dorthe Ejersbo (Denmark)
Secretary, European Advisory Committee for Cytology September 30, 2006